Background: Rest is critical to healing, yet a child’s sleep during an inpatient hospital admission is often disrupted. One such disruption is oral medication administration, which is commonly scheduled around the clock (q6h, q8h, q12h) by default, despite comparable efficacy during waking hours. Previous studies suggest that flexible medication times help inpatients sleep longer and that convenience of scheduling increases adherence to medication. Prior quality improvement (QI) efforts by our group to limit overnight blood pressure checks successfully improved sleep in pediatric inpatients. However, oral medication administration remains a top disruptor to hospitalized children’s sleep, as reported by caregivers. This study aimed to decrease the disruptiveness of oral medication administration to patient sleep by utilizing electronic health record (EHR) changes and interprofessional education to increase the proportion of oral antibiotic orders with sleep-friendly administration schedules.
Methods: EHR order screens for amoxicillin, amoxicillin-potassium clavulanate, clindamycin, and cephalexin were modified to default to sleep-friendly administration schedules (QID, TID, BID), rather than around the clock administration schedules (q6h, q8h, q12h), for hospitalized pediatric patients. Education sessions on the importance of sleep-friendly administration schedules targeted nurses and residents. Session effectiveness was evaluated using a Likert scale survey that asked participants to agree or disagree with statements regarding the disruptiveness of different oral medication administration schedules to sleep pre- and post-education. Antibiotic utilization reports tracked the use of sleep-friendly administration schedules.
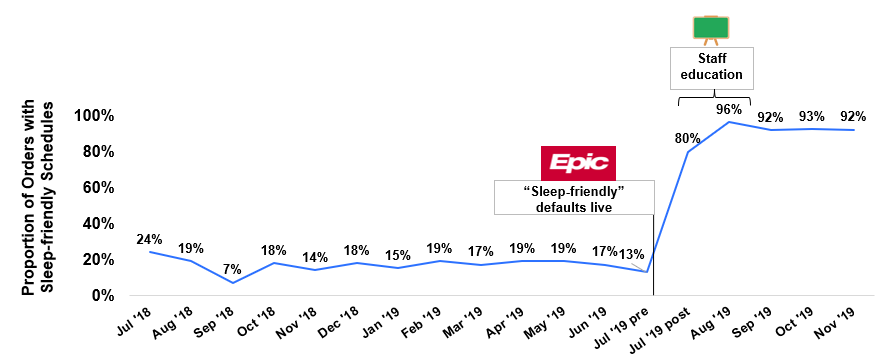
Results: 63% (51/81) of pediatric residents and 76% (68/90) of nurses completed a post-education session survey. Following the sessions, a significant improvement was seen in residents’ and nurses’ agreement that oral medications scheduled q6h, q8h, and q12h cause sleep disruption (resident: 73% pre, 92% post, p=0.01; nurse: 62% pre, 78% post, p=0.04). After receiving education regarding the intervention, residents and nurses reported a significantly higher level of agreement that oral medications are optimized for sleep in the hospital (resident: 22% pre, 55% post, p<0.001, nurse: 12% pre, 35% post, p=0.002). In the four months post-intervention, the proportion of orders with sleep-friendly administration schedules has shown a statistically significant increase (pre-intervention (July 2018-2019): 17% [172/1,014 orders], post-intervention (July-November 2019): 92% [210/229 orders], p<0.001).
Conclusions: The high adoption rate seen with this intervention highlights the impact quality improvement efforts via EHR modifications and clinician education can have on hospital practice and patient care. Interprofessional collaboration throughout the design and implementation process was critical to a smooth uptake of the intervention and contributed to its positive reception. Future work will include continued EHR order usage data collection and surveys of pediatric patient caregivers regarding the disruptiveness of medication administration to inpatient sleep.