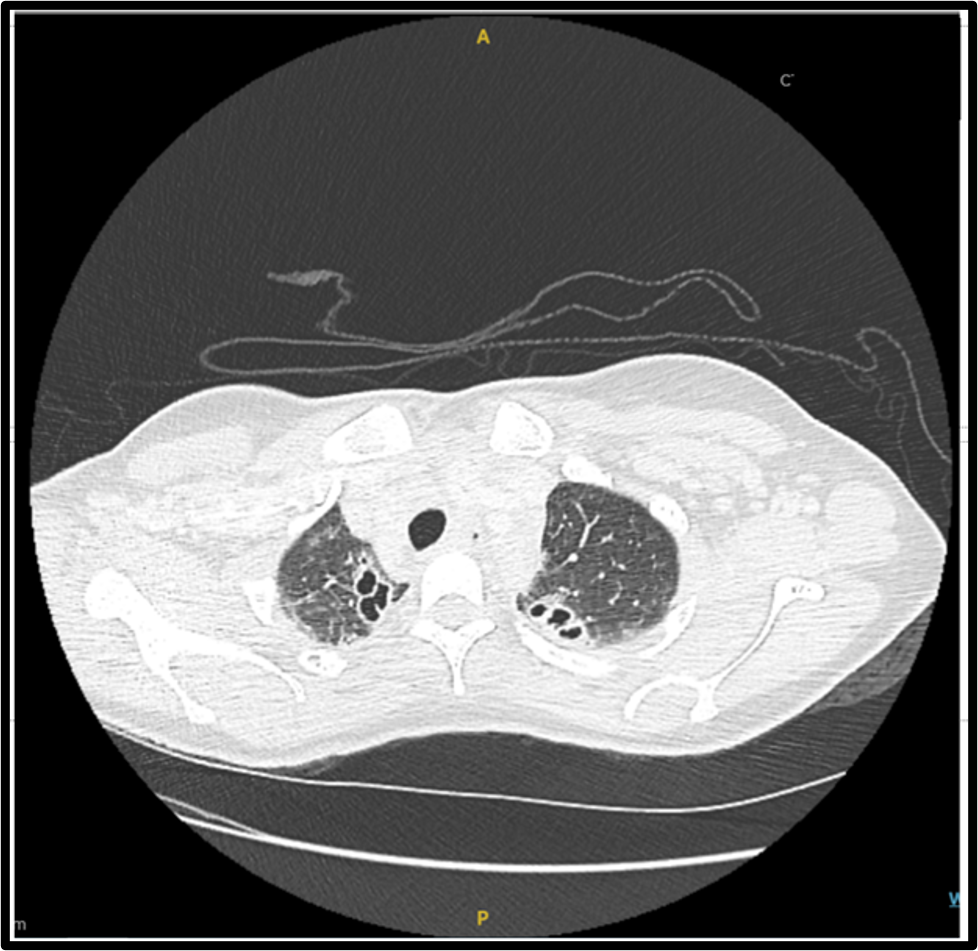
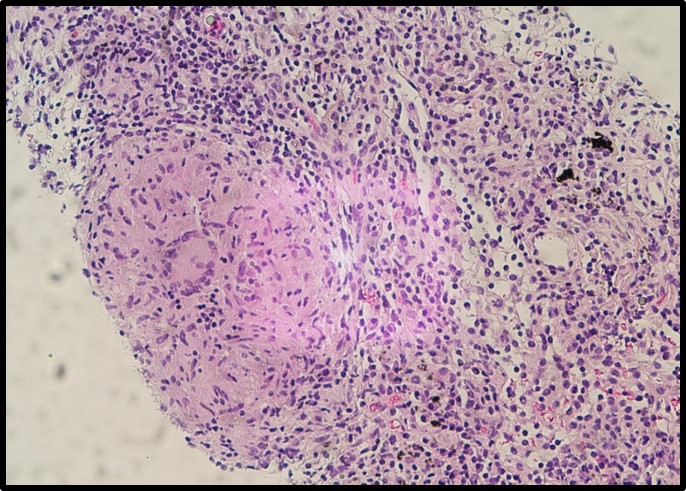
Case Presentation: A 33-year-old female with a history of alcohol use and rheumatoid arthritis presented with a 2 day history of sharp, peri-umbilical and left upper quadrant (LUQ) pain. She also reported one month of fevers, night sweats, unintentional 10 Lb weight loss, and a non-productive cough without hemoptysis. She underwent a dental extraction for an odontogenic infection 8 weeks prior. She denied current treatment with biological agents, sick contacts, recent travel, or any family or personal history of malignancy. On examination, vital signs were stable with palpable and tender cervical lymphadenopathy (LAD) and tenderness to palpation of epigastrium and LUQ. Workup revealed leukopenia (3.18 K/uL), transaminitis (ALT 91 IU/L; AST 196 IU/L; ALP 392 IU/L), and elevated lipase (434 IU/L). CT of chest/abdomen/pelvis showed enlarged cervical, supraclavicular, mediastinal, hilar and retroperitoneal lymph nodes (LN) and a new bilateral upper lobe thick walled irregularly shaped cavitary lesions. There was no evidence of pancreatitis. Given the history and findings, there was a concern for lymphoma. Infectious disease, Hematology and Pulmonology were consulted. Blood and fungal cultures were negative. Serial morning sputum samples were negative for acid-alcohol fast bacilli. ANA, ANCA, RF, and anti-CCP were unrevealing. HIV serology was unreactive. ACE level and IgG4 levels were normal, and EBV PCR was negative. Bartonella serologies returned equivocal (IgM < 1:16, IgG 1:128). Flow cytometry was negative, and no blasts were seen on peripheral smear. A bronchoscopy with bronchoalveolar lavage was performed. Cultures returned positive for Actinomyces odontolyticus. Cytology was negative for malignancy. Histopathologic examination of an axillary LN biopsy showed reactive changes with granulomatous inflammation. The patient was started on IV Penicillin G and discharged on Augmentin. Two months after discharge, a follow-up CT chest and abdomen showed complete resolution of the lung cavitations and LAD.
Discussion: A. odontolyticus is a gram-positive anaerobic bacteria found mainly in the oral cavity and digestive tract. It causes actinomycosis, a chronic granulomatous disease. A.odontolyticus has been identified as an emerging bacterium, with only a few cases reported of thoracic, abdominal, and central nervous system involvement with signs and symptoms that overlap with other infectious and neoplastic conditions, making it difficult to diagnose, as in our patient. Alcohol consumption and recent periodontal disease were the risk factors for the infection in this case, but immunosuppression and malignancy have also been described. Gram staining and pathology are more sensitive than culture for diagnosing A. odontolyticus. The preferred therapy is Penicillin G for 2-6 weeks; however, given reports of complications and invasive infections, immunocompromised patients might benefit from extended treatment with oral antibiotics for 6-12 months.
Conclusions: A. odontolyticus infection represents a clinical challenge and highlights the importance of a multidisciplinary approach when the initial evaluation remains inconclusive to avoid delayed diagnosis and increased morbidity and mortality.