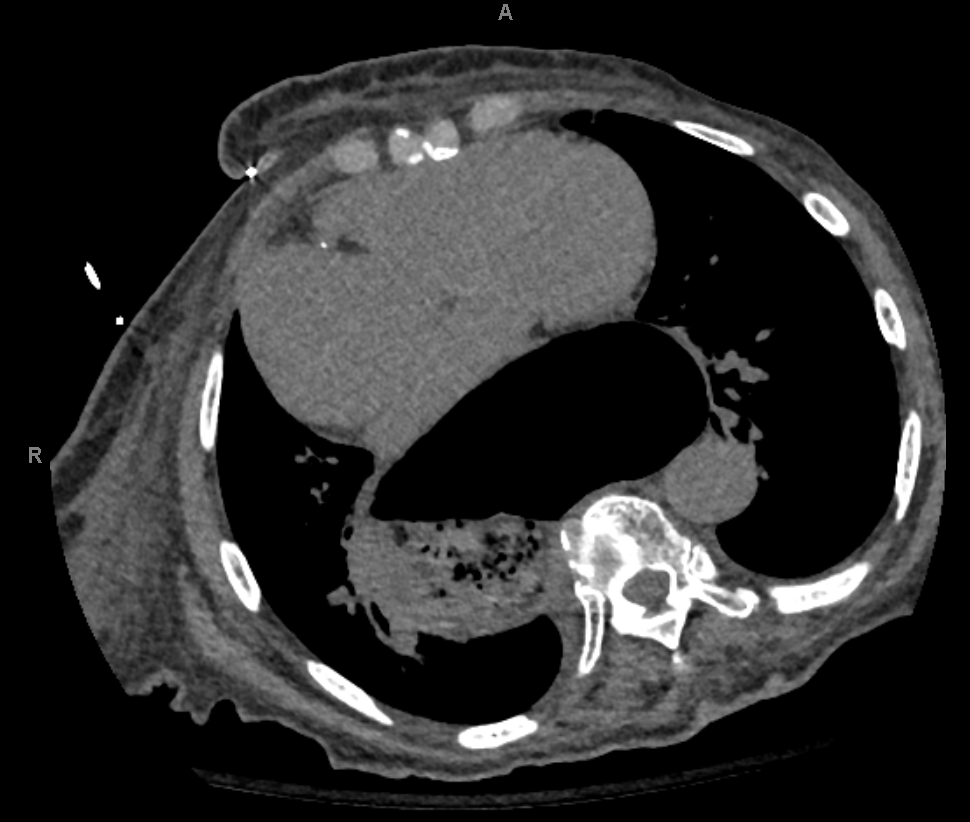
Case Presentation: A 99-year-old female presented to the emergency department due to new onset, post-prandial abdominal pain, nausea, and vomiting. History was significant for atrial fibrillation (AFib), heart failure with preserved ejection fraction (HFpEF), diabetes, and hypertension. Physical exam was significant for chronic bilateral lower extremity edema without JVD or rales. On admission, her electrocardiogram showed AFib with low voltage and no signs of active or prior ischemia. Lab work revealed an elevated high sensitivity troponin T of 27 (< 19 ng/L), an N-terminal prohormone brain natriuretic peptide (pro-BNP) of 3,507 pg/mL (>75yr age normal < 450pg/mL), and a creatinine of 1.62 mg/dL (patient baseline 0.7 - 0.8mg/dL). A chest X-ray and CT scan identified a large type III hiatal hernia with diffuse cardiac compression.A nasogastric tube was placed for decompression. Twelve hours later, an echocardiogram revealed biatrial and right ventricular dilation, pulmonary arterial pressure of 56mmHg, and moderate to severe tricuspid regurgitation. She had worsening right sided heart function compared to her prior echo consisting of no chamber enlargement, pulmonary arterial pressure of 40mmHg, and mild tricuspid regurgitation. After 48 hours of suction and IV fluids to resolve her hypovolemic prerenal AKI, a barium study was performed without any signs of obstruction, the patient progressed to a PO diet, and was later discharged. Given the lack of volvulus or obstruction, the patient’s age and preference, surgery was deferred.The patient also had two recent, prior hospitalizations for dyspnea where she was initially diagnosed with AFib and HFpEF and received symptomatic management. An extensive hiatal hernia was present on chest X-ray at those times as well, although no decompressive intervention was performed.
Discussion: Hiatal hernia types II-IV are paraesophageal hernias of varying degrees and encompass 5-15% of hiatal hernia cases. Gastrointestinal symptoms can range from gastroesophageal reflux disease to obstruction, ischemia, or volvulus of the hernia sac. As seen in prior case reports, severe hernias can precipitate cardio-respiratory symptoms including acute coronary syndrome, arrhythmias, syncope, dyspnea, and congestive heart failure. Patients with hiatal hernias have an increased frequency of AFib due to external pressure placed on the left atria and pulmonary veins. Additionally, compression of inferior pulmonary veins can precipitate pulmonary edema, pleural effusions, diastolic dysfunction, and right sided heart dysfunction. This patient’s initial AFib and HFpEF diagnoses were likely due to the compressive mass effect of her hiatal hernia. Her more recent heart failure work up including an increasing pulmonary arterial pressure with worsening valvular dysfunction and elevated pro-BNP were the result of her enlarging chronic hiatal hernia without an overt CHF exacerbation. Earlier recognition, decompression, and/or surgical repair may have prevented her cardiac manifestations. This case emphasizes the importance of considering hiatal hernias as a reason for cardiac abnormalities and disease, specifically when temporally related to a meal.
Conclusions: Hiatal hernias can remain asymptomatic or present as a wide range of multi-organ system symptoms including cardio-respiratory due to compressive mass effect. It is important to be prudent and consider it as an imitator and instigator of cardiac disease, one that may be reversible with appropriate interventions.