Case Presentation: A 57-year-old woman with type 1 diabetes on insulin pump and hypertension presented to the ED with abdominal pain with associated nausea/vomiting and shortness of breath for one day. She reported her insulin pump has been malfunctioning for several days. She denied fever/chills, chest pain, or diarrhea. She denied any toxic habits.Vital signs were BP 104/52 mmHg, HR 124/min, RR 20/min, afebrile and SpO2 99% on RA. Physical exam showed a patient in moderate distress due to dry-heaves, tachycardia but otherwise normal cardiac and lung exam. Abdomen was diffusely tender to palpation but soft without guarding or rebound.
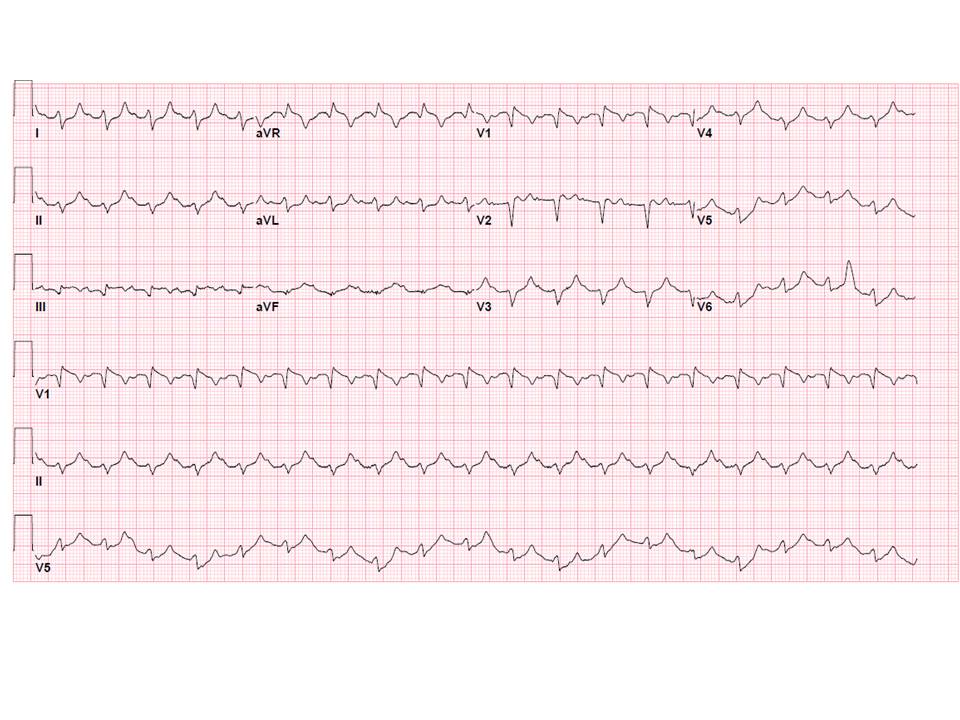
Venous blood gas revealed pH 6.94, pCO2 24 mmHg, lactate 3.4 mmol/L. Other laboratory tests included Na 132 mmol/L, K 7.4 mmol/L, CO2 <5 mmol/L, BUN 42 mg/dL, Cre 1.5 mg/dL, incalculable anion gap, glucose 927 mg/dl, WBC 14.4 K/uL with 86% neutrophils, ketonuria and glycosuria. EKG showed sinus tachycardia to 117/min, incomplete right bundle branch block (iRBBB), Q waves in III, AVF, V1, with non-specific T-wave changes (figure 1). There was no available prior EKG. Chest X-ray showed enlarged cardiac silhouette.
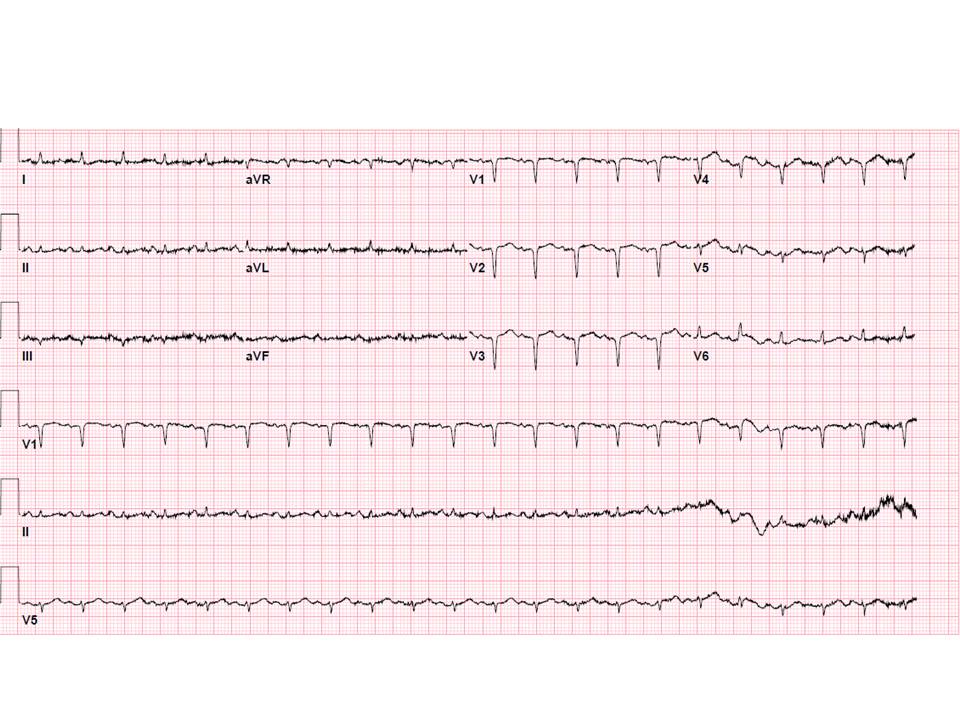
Patient was initiated on intravenous fluids and continuous insulin infusion and admitted to medical ICU overnight for management of severe diabetic ketoacidosis (DKA) suspected due to insulin pump malfunction. Serial laboratory tests showed improvement in acidosis and glucose levels, however she had persistent nausea. Next morning, troponin was sent for workup of DKA, which returned elevated at 127.6 ng/mL. Repeat EKG showed sinus tachycardia with resolved iRBBB but with new Q waves in V2-4 (figure 2), concerning for acute anterior infarct. She was immediately initiated on dual antiplatelets (DAPT), heparin, and statin, and underwent cardiac catheterization, which showed triple vessel disease with total occlusion of mid left anterior descending artery. She was continued on maximal medical therapy except for DAPT to be evaluated for surgical revascularization. She successfully underwent coronary artery bypass graft on hospital day 7.
Discussion: This case demonstrated a delay in appropriate workup and treatment for acute coronary syndrome (ACS) in a type 1 diabetic woman who presented with diabetic ketoacidosis (DKA).
One-third of patients with acute coronary syndrome (ACS) present with no chest pain. Atypical presentation is more likely in elderly, diabetic, and female patients. In these populations, the threshold for EKG and cardiac biomarkers should be lower.
Although male sex is associated with much increased ACS morbidity and mortality, type 1 diabetes is an exception. A recent large study with over 400,000 patients in UK showed that compared with people without diabetes, women with type 1 diabetes had more than eight times the risk of ACS, while hazard ratio of men was about three. In type 1 diabetes, female sex is associated with excess relative risk for ACS.
As delayed recognition and treatment of ACS can lead to significant increase in mortality, providers must be aware that women with type 1 diabetes have significantly high risk of developing ACS in the setting of frequent atypical symptoms.
Conclusions: Women with type 1 diabetes are at significantly high risk for acute coronary syndrome. Careful review of EKG and low threshold for cardiac biomarkers are imperative as they often also have atypical presentations.