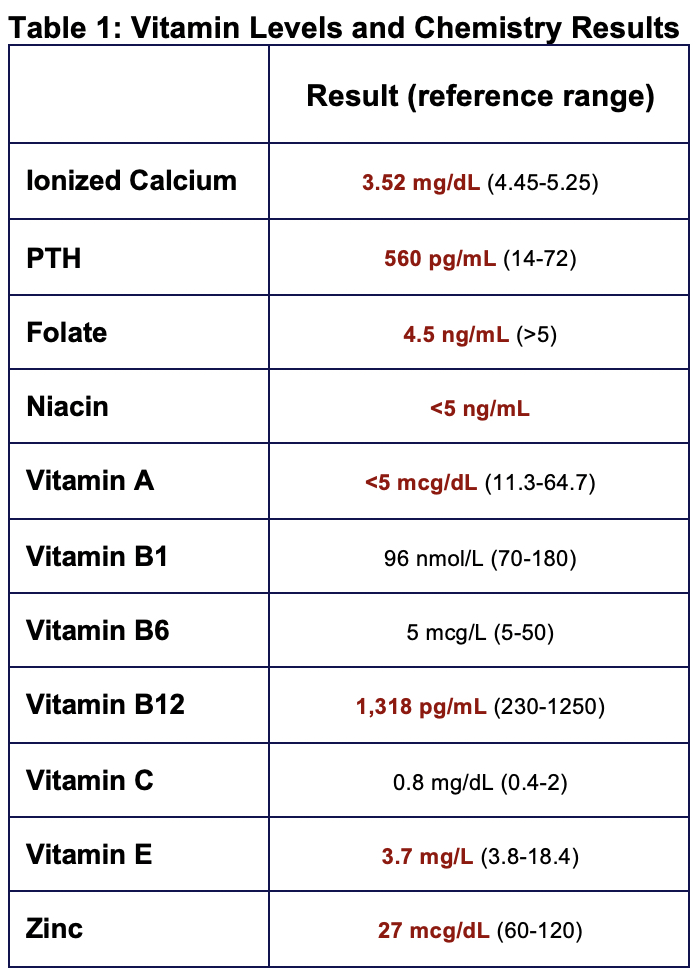
Case Presentation: A 3-year-old immunized male, with a history of atopic dermatitis and anaphylactic dairy allergy, was brought to the ER due to refusal to bear weight for one month. There was no trauma, fevers, or recent sick symptoms. He had a severely restricted diet of potato products and breast milk. On exam, he was well appearing with eczematous lesions on the dorsal aspects of his hands, feet, and face, along with frontal bossing. He had a 2/6 systolic murmur, and non-focal respiratory and abdominal exam. He had full range of motion and genu varum deformity of bilateral lower extremities without erythema or tenderness. Labs revealed serum calcium of 6.5 mg/dL, mild acidosis of CO2 15 mmol/L, alkaline phosphatase of 1,978 units/L. Vitamin D was 6 ng/dL (Table 1). Normal blood counts and inflammatory markers. X-ray (XR) of bilateral femurs demonstrated diffuse osteopenia with widening and fraying of the distal metaphyses of the femurs and proximal tibias. The diagnosis of calcipenic rickets was made and he was started on standard therapy. On day 3, he developed fever to 40.1 degrees C. Respiratory pathogen panel and complete blood count negative for infection. His fever resolved within 24 hours. However, on day 7, he became febrile and complained of right arm pain. Repeat labs revealed CRP 43.5, ESR 66 but no elevated WBC count. An XR of his right humerus demonstrated mild soft tissue edema and MRI showed a right shoulder joint effusion with findings of synovitis and surrounding myositis (Figure 1). Aspiration revealed acute suppurative septic arthritis with 29,206 cells/Cumm nucleated cells. Synovial cultures were positive for methicillin susceptible staphylococcus aureus (MSSA) and blood cultures positive for MSSA within 19.9 hours.
Discussion: Our patient’s unique presentation of calcipenic rickets and atopic dermatitis with subsequent development of MSSA septic arthritis and bacteremia highlight the immunomodulatory properties of vitamin D and the possible immunologic effects of treatment of rickets and various vitamin deficiencies. In addition to the role of vitamin D in skin immunomodulation, decreased serum concentrations of vitamin D have been linked to disruption of important pleiotropic roles in immune function, including respiratory compromise and infection in the pediatric population. It is possible that as bone mineralization increases during vitamin and mineral supplementation in rickets treatment, increased bone perfusion could lead to elevated risk of osteomyelitis and septic arthritis due to hematogenous spread of bacteria. As well this, cases have been reported in patients with atopic dermatitis developing systemic complications including bacteremia, septic arthritis, osteomyelitis, and endocarditis. Most of these infections are caused by MSSA, and up to 90% of patients with atopic dermatitis have MSSA colonization. Our patient, having required frequent IV placements, lab draws, and infusions, was at increased risk given concurrent eczema and skin breakdown and frequent breaches of skin.
Conclusions: In summary, increased bone perfusion during rickets treatment, skin barrier breakdown secondary to vitamin D and other micronutrient deficiencies and repeated IV placements are all mechanisms through which rickets patients may be at increased risk for septic arthritis and other systemic infections. We hope that this case helps elucidate potential associations between acute bone/joint infection and rickets treatment and inform clinical decision making in similar patient presentations.