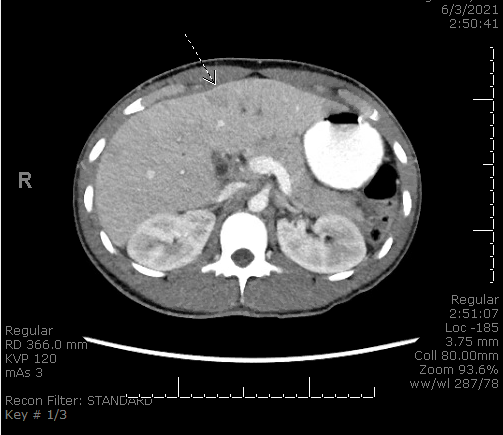
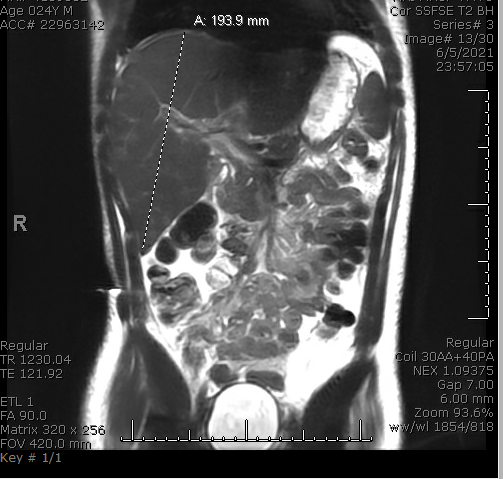
Case Presentation: A 24-year-old male with a history of acute pancreatitis three months prior, presented with sharp peri-umbilical and right upper quadrant abdominal pain for three weeks. He endorsed fevers, rigors, jaundice, nausea, vomiting, poor appetite, and dark colored urine. He denied hematemesis, melena or hematochezia. He had intermittent alcohol use but no illicit drug or tobacco use. On arrival, he was septic with tenderness on abdominal palpation. He had a leukocytosis, hyperbilirubinemia, transaminitis, elevated alkaline phosphatase and lipase levels. Imaging demonstrated intrahepatic biliary dilation, gallbladder inflammation, concern for choledocholithiasis with obstructing stone, and colonic wall thickening at the hepatic flexure. There was also bilobar portal venous thrombophlebitis with areas of hypoattenuation. He was started on broad-spectrum antibiotics and resuscitated with fluids. An urgent ERCP demonstrated no pus or obstruction, but he required biliary sphincterotomy with sludge clearance, percutaneous cholecystostomy drain placement and ventral pancreatic duct stenting. He was started on a heparin drip. A hypercoagulable workup was unremarkable. Four days post-procedure, he developed worsening hyperbilirubinemia and large melanotic stools. Repeat ERCP demonstrated bleeding at the sphincterotomy that was treated. He was resumed on heparin and transitioned to apixaban when bleeding resolved. The patient also had a polymicrobial bacteremia and discharged on oral Levaquin and Flagyl. His liver function improved and anticoagulation was stopped at three months later.
Discussion: The incidence of portal vein thrombosis (PVT) among patients without cirrhosis is unclear. It may account for 5 to 10 percent of patients with portal hypertension in developed countries and up to a third in developing countries[1,2]. Etiology is thought to be due to inherited or acquired prothrombotic states[3]. No apparent cause is identified in more than 25 percent of patients [4-6]. Inherited causes are standard hypercoagulable states (Factor V Leiden, protein c deficiency, etc.) Acquired causes include surgery, inflammatory bowel disease, trauma, or in our case, abdominal infection such as pancreatitis/cholangitis. A proposed pathogenesis of PVT in pancreatitis/cholangitis may be venous compression by a pseudocyst and an imbalance between blood coagulation and fibrinolysis [7]. Without diagnosis and treatment, complications such as intestinal ischemia, portal hypertension, and portal cholangiopathy can occur. Our patient was found to have a bilobar portal vein thrombophlebitis that was treated with anticoagulation in a man with recurrent, non-necrotizing, non-alcoholic pancreatitis. Although our patient did not require thrombectomy or balloon dilation for complete reperfusion, he did develop thrombocytopenia from the clot and melanotic stools. The patient successfully underwent a repeat ERCP with cauterization of active bleeding from the ampulla of biliary sphincterotomy site.
Conclusions: We present a rare case of PVT in a patient with recurrent pancreatitis and cholangitis requiring a stent and anticoagulation, that led to bleeding. Our case reminds physicians to always suspect and investigate further when a patient’s symptoms continue to persist despite standard therapy as improvement may be hindered by other active ongoing pathology. A timely diagnosis and therapy are quintessential to prevent rapid deterioration or even death in severe abdominal infections.