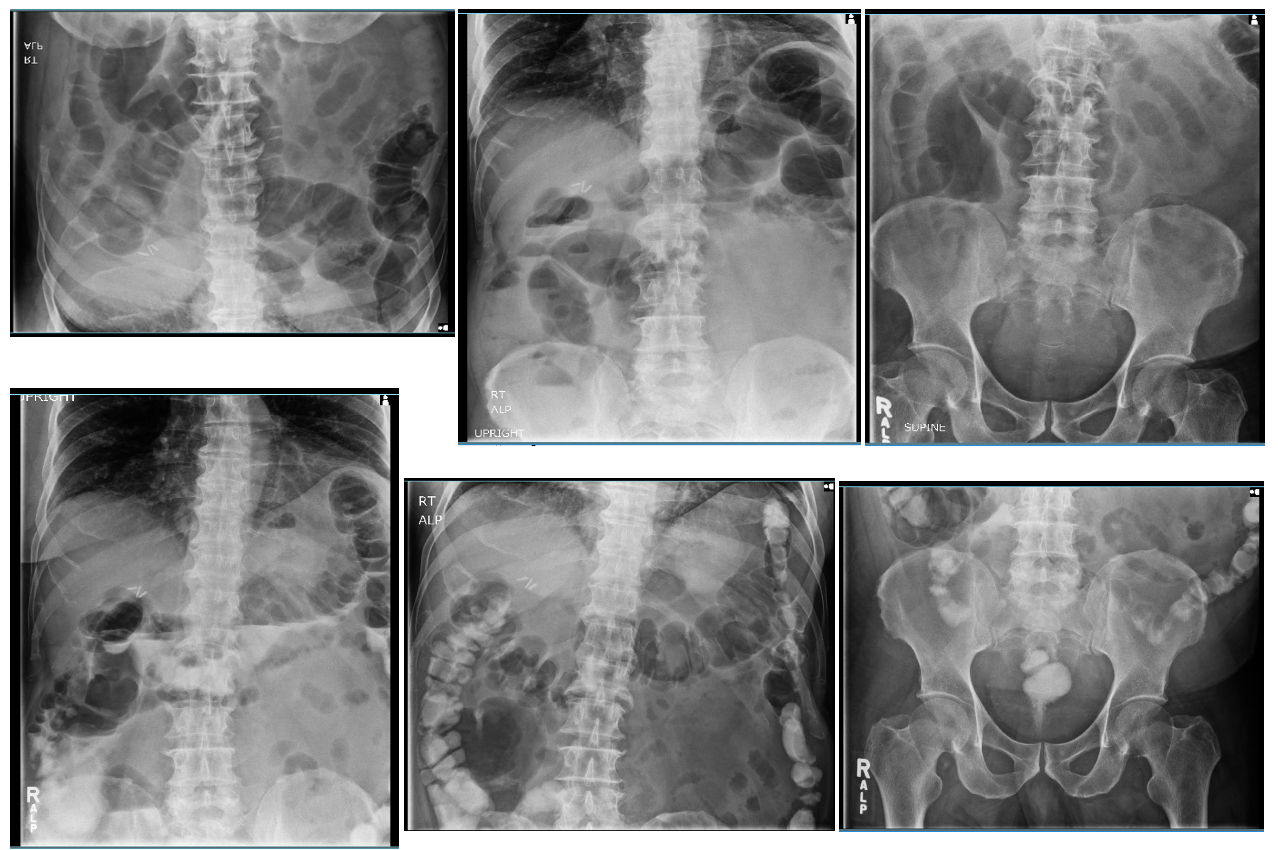
Case Presentation: A 74-year-old man presented to our rural hospital for evaluation of three days of right flank and abdominal pain with constipation. Initial examination and workup were unremarkable, and the patient was discharged on laxative therapy. Two days later, the patient returned with worsening abdominal discomfort, constipation, and a painful rash to the right flank. The patient had abdominal distension with sluggish, hypoactive bowel sounds. Dermatological exam revealed a maculopapular rash with vesicles in various stages of healing on an erythematous base across the right flank in a dermatomal distribution at the levels of L1 to L3. (figure 1). Acute abdominal x-ray series revealed early/partial small bowel obstruction (SBO). (figure 2) A complete SBO would necessitate transfer for surgical consultation. At our rural hospital, the nearest major hospital is over 100 miles away, necessitating costly aircraft transport for nearly all patient transfers. The patient was admitted for conservative management of possible early/partial SBO and was continued on laxatives in conjunction with antiviral therapy. Repeat imaging with gastrografin, which revealed improvement in the small bowel (figure 2) two days later, and after four days, the patient was stable for discharge.
Discussion: Herpes zoster results from reactivation of varicella zoster virus (VSV) infection earlier in life. VZV remains dormant in sensory neuron ganglia until reactivation, most often after age 65 (1). Herpes zoster infection classically presents with neuralgia and vesicular rash, however many complications exist due to potential involvement of autonomic ganglia (2). There have been several documented cases of colonic pseudo-obstruction or Ogilvie syndrome resulting from herpes zoster infection (3,4,5). The most prominent hypothesized pathogenesis is that primary infection of the enteric nervous system with VZV leads to direct neuronal injury to the muscularis propria of the small intestine upon reactivation as herpes zoster. Most documented cases demonstrated good outcomes with relatively quick resolution of symptoms after first line treatment of herpes zoster with adjunctive management of pain and constipation (6). In this case, the presence of a dermatomal herpetic rash helped determine the etiology of this patient’s intestinal paresis, allowing us to initiate appropriate inpatient therapy.
Conclusions: Here we describe a bounce back case of a rare manifestation of zoster pseudo-obstruction that is further complicated by management in the rural hospital setting where surgical intervention is not accessible and would require patient transfer via aircraft.Visceral neuropathy with intestinal paresis is an uncommon complication of herpes zoster which can lead to life-threatening complications such as intestinal pseudo-obstruction and SBO. In this case, because we suspected herpes zoster infection was the underlying cause of early/partial SBO, we were able to avoid costly interventions. Awareness of herpes zoster related autonomic dysregulation is important, as recognition of a zoster-induced paresis allows providers to optimize treatment.