Background: Alcohol use disorder (AUD) is the most prevalent substance use disorder, but most patients with AUD do not receive evidence-based medications for AUD (MAUD), including naltrexone or acamprosate. Inpatient addiction consult services (ACS) may offer an opportunity to start medical treatment for hospitalized patients with AUD, but it is unknown if ACS are associated with increased likelihood of treatment and/or improved outcomes. We sought to determine the association between an ACS consultation and provision of MAUD, and post-discharge outcomes.
Methods: The intervention was ACS consultation which consisted of a multidisciplinary team including a board-certified addiction medicine attending physician, an addiction medicine fellow, and peer advocate. We used a retrospective propensity score-matched historical control design to evaluate the effect of ACS consultation for hospital admissions with a primary or secondary diagnosis of AUD. Each admission with AUD who received an ACS consult was matched with a control admission from the historical, consult-unavailable time period. The propensity score model was a non-parsimonious 29-variable model including demographic, clinical and admission-level covariates. The primary outcomes were provision of MAUD during the admission and prescription for MAUD at discharge. Secondary outcomes included: patient-directed discharge, 7-day and 30-day readmission, and 7-day and 30-day post-discharge ER visit. Unadjusted and adjusted associations between consultation and each of the outcomes were determined using univariable and multivariable logistic regression, and Cox-proportional hazards models.
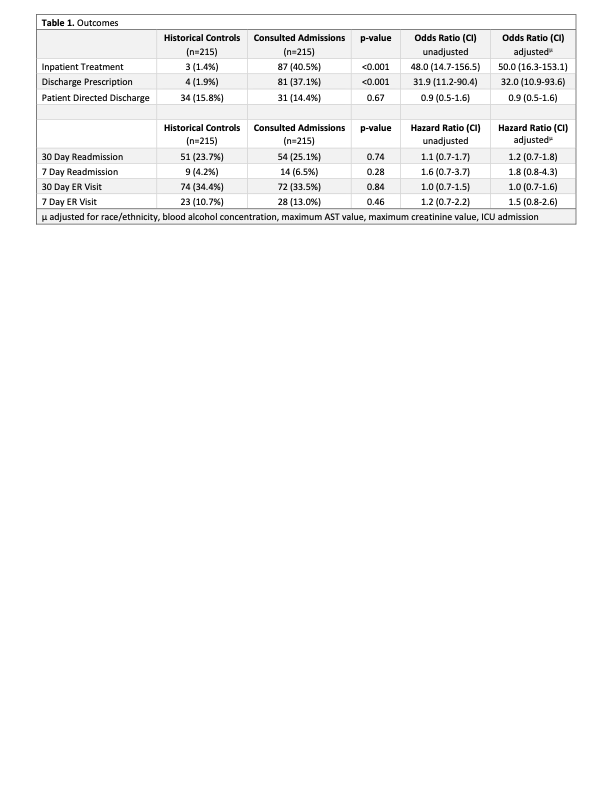
Results: Among hospitalizations with a primary or secondary diagnosis of AUD, there were 215 admissions who received an ACS consultation matched with 215 historical controls yielding a study sample of 430 admissions. Admissions who received an ACS consultation were significantly more likely to receive inpatient MAUD, compared to historical controls in both unadjusted (40.5% vs 1.4%; ORunadj 48.0 [CI 14.7-156.5]) and adjusted (ORadj 50.0 [CI 16.3-153.1]) analyses. There was also a significantly greater likelihood among ACS consulted admissions to receive a prescription for MAUD at discharge compared with historical controls, in both unadjusted (37.1% vs 1.9%; ORunadj 31.9 [CI 11.2-90.4]) and adjusted (ORadj 32.0 [CI 10.9-93.6]) analyses. However, ACS consultation was not associated with reduced patient-directed discharge, 7-day or 30-day readmission, or 7-day or 30-day post-discharge ER visit.
Conclusions: ACS was associated with a large increase in inpatient provision of MAUD and MAUD prescription at discharge when compared to propensity-matched historical controls. These findings provide compelling evidence for the benefit of an ACS in hospitals which have a high prevalence of patients with AUD.