Background: Despite significant efforts, sepsis remains a common cause of hospital readmissions nationwide, and patients are often readmitted within two weeks after their index admission. Not only are patients who develop sepsis often chronically debilitated, sepsis can lead to systemic sequelae that includes functional deconditioning, cognitive impairment, sepsis-induced immunosuppression and inflammation, and cardiovascular risks. This constellation of symptoms is referred to as Post-Sepsis Syndrome (PSS). Patients with PSS often have difficulty adhering to instructions for self-care, completing medical follow-up appointments, and managing Activities of Daily Living.
Purpose: We developed a comprehensive and interdisplinary transition of care program to enhance the discharge process and extend care delivery to include the vulnerable 2-week post-discharge period for patients discharged with a diagnosis of sepsis.
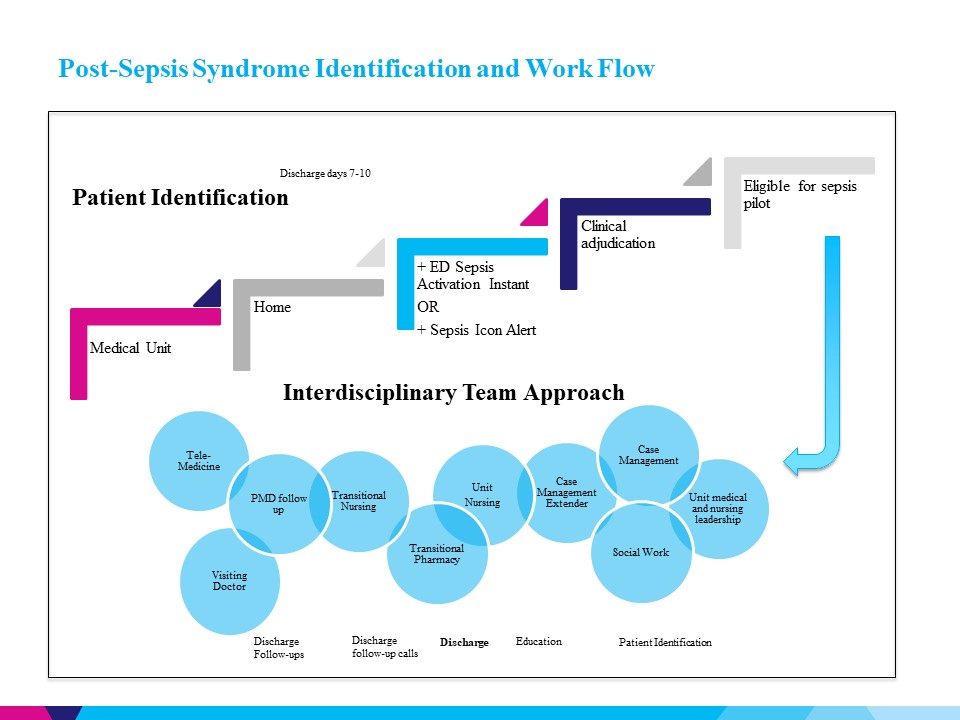
Description: The PSS team is an interdisciplinary team that includes the medical unit’s case manager (CM) and CM extender, nurse manager, social worker, clinical pharmacist, medical director, transitional care (TC) nursing staff, visiting doctor (VD) service, and tele-medicine service. Patients are screened into the program by the CM and are eligible if they are both diagnosed with sepsis at any point during their hospitalization and are planned for discharge to home. This is a two-step process where the sepsis diagnosis is confirmed by the provider of record within 1-2 days prior to hospital discharge and the social worker helps to screen patients being discharged home for any post-acute care needs to coordinate the appropriate services. After confirmation, the CM extender introduces the program to the patient and coordinates outpatient follow-up appointments to patients/caregivers. In addition, the CM extender facilitates patient enrollment in the Tele-Medicine and Visiting Doctor programs if appropriate. Patients enrolled in our PSS program receive enhanced sepsis education from the nursing team, including information on the expected PSS symptoms and other symptoms of concern. The unit pharmacist completes medication reconciliation and provides education prior to discharge. After discharge, the TC nursing staff contacts the patient at days 1-3 and again at days 7-10 to reinforce education, treatment, and adherence to the follow-up plan of care. On hospital discharge days 4-6, the discharging pharmacist conducts a follow-up call using a standardized script to address any medication issues or concerns. If patients reside within the VD service area, they receive a home visit by a physician within 7 days post-discharge. During the 30-day post-discharge period, patients are also able to initiate a virtual appointment with a provider. At any point, clinical concerns that arise may be escalated to the members of the discharging team, which includes the primary attending, resident, and social worker.
Conclusions: Patients with sepsis are at high risk of Post-Sepsis Syndrome. This may cause cognitive impairment and functional deconditioning which leads to suboptimal self-care and adherence to medical follow-up post-discharge. Extending the care from the inpatient setting to two weeks post-discharge using a comprehensive and interdisciplinary team approach may help mitigate the risk of readmission, morbidity, and mortality for septic patients at increased risk for developing PSS.