Background: Administrative harm (AH), defined as negative consequences arising from administrative processes and decisions within healthcare, is pervasive in medicine, yet poorly understood and described.
Methods: We sought to explore common AHs experienced by hospitalist clinicians, administrative leaders, researchers, and patient and family advisory council members that were part of two national consortiums for hospitalists including a national research network and a national society special interest group for academic leaders. We aimed to understand the challenges that exist in identifying and measuring AH and to identify potential approaches to mitigate AH. Ten semi-structured virtual focus groups were held with 41 unique individuals from 32 different organizations. Rapid qualitative methods including templated summaries and matrix analysis were applied. A brief 12-question survey was also conducted.
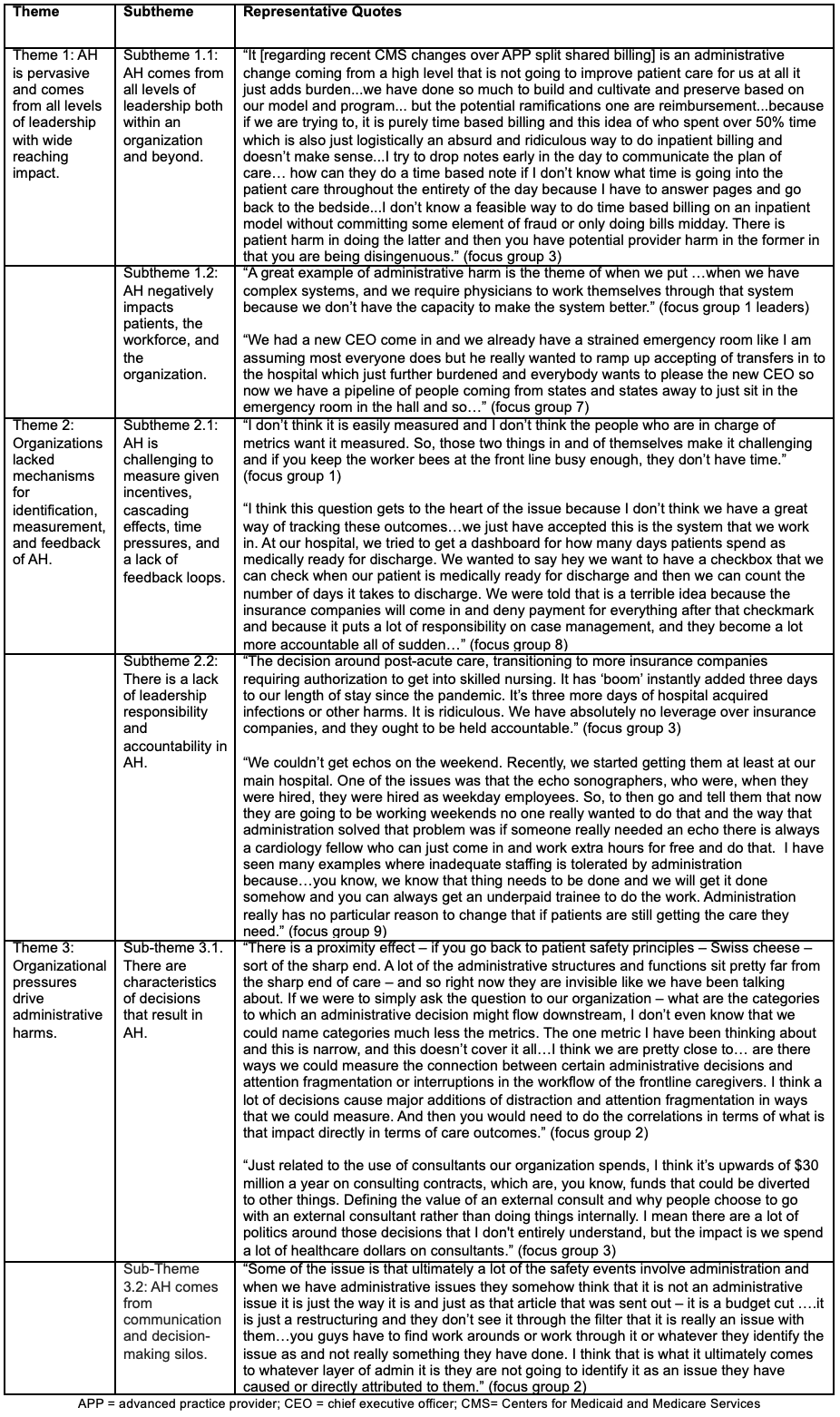
Results: Ten semi-structured virtual focus groups were held with 41 individuals from 32 different organizations on June 13th, 2023 and August 11, 2023. Thirty-two participants completed the survey (78% response rate). Mean years of practice was 14 with a standard deviation (SD) of 6. Mean percent clinical effort of participants was 53% (SD of 24). Of those who filled out the survey, 32 (86.5%) were physicians, 4 (10.8%) were administrative professionals, and 1 (2.7%) was an advanced practice provider (APP). Seventeen participants (46%) considered themselves leaders. Almost 60% of the participants were “not at all” or “very little familiar” with the term AH, 88% felt that “collaboration between administrators and clinicians is crucial for reducing AH”, and that 81% had “personally participated in a decision that led to AH”. We identified three main themes with subthemes (Table): (1) AH is pervasive and comes from all levels of leadership and impacts patients, the workforce, and organizations. (2) Organizations lacked mechanisms for identification, measurement, and feedback noting that AH is challenging to measure and that there are perverse incentives to not measure it. Current leadership structures often lack ownership of downstream problems in part because of decisional distancing and the normalization of these harms. (3) Organizational pressures were recognized as drivers of administrative harms and that there were specific characteristics of decisions that were noted to result in AH including decision-making silos. Our work also yielded a conceptual model for understanding AH (Figure). Many ideas were proposed as solutions including: (1) understanding and defining AH such as labeling the harms and developing a conceptual model of AH, (2) building collaborative cultures and psychological safety in workplaces including avoiding “us” vs “them” mentality and promoting transparency and accountability in decision making, (3) utilizing decision making frameworks and a commitment to evaluate decision making including conducting decision making “time-outs” and ensuring more clinicians with business training, (4) utilizing measurement and data strategies including using quantitative and qualitative data to measure outcomes of decisions, and (5) reporting and learning including building AH reporting structures similar to patient safety reporting systems and developing multidisciplinary review processes.
Conclusions: AH is pervasive and has wide reaching impacts, is challenging to identify and measure, yet there are many opportunities to mitigate it.