Case Presentation: A 60-year-old previously healthy female presented with a two-week history of intermittent fever with non-pruritic rash, generalized myalgias and arthralgia, weakness, and chest pain.
Her exam revealed temperature of 39.3 degrees Celsius, anterior chest tenderness to palpation, diffuse salmon-colored maculopapular rash at bilateral extensor surfaces of upper extremities, and multiple coalescing annular rash at the left lower back with central clearing.
Laboratory studies were notable for the following: WBC 2.2 with ANC of 1232, Hgb 8.9, Hct 27, MCV 87, RDWC 14.3, Plt 41, K 2.5, Cr 1.45, phosphorus 1.1, AST 310, ALT 79, total bilirubin 1.3, direct bilirubin 0.9, CK 466, LDH 2365, haptoglobin <8, ferritin >80000, fibrinogen 139, fasting triglycerides 371, lactate 3.1, negative Troponin I with repeat. Peripheral blood smear revealed hypoproliferative normocytic normochromic anemia with no increase in schistocytes, and neutrophils with mild toxic changes and left shift.
The EKG revealed sinus tachycardia at 117 beats/minutes with left axis deviation. The CXR demonstrated congestion of the central pulmonary vasculature with interstitial opacities bilaterally. Retroperitoneum ultrasound revealed mildly enlarged spleen. A CT angiography of chest, abdomen, and pelvis revealed nonspecific mild centrilobular nodules in the right lung. TTE was unremarkable.
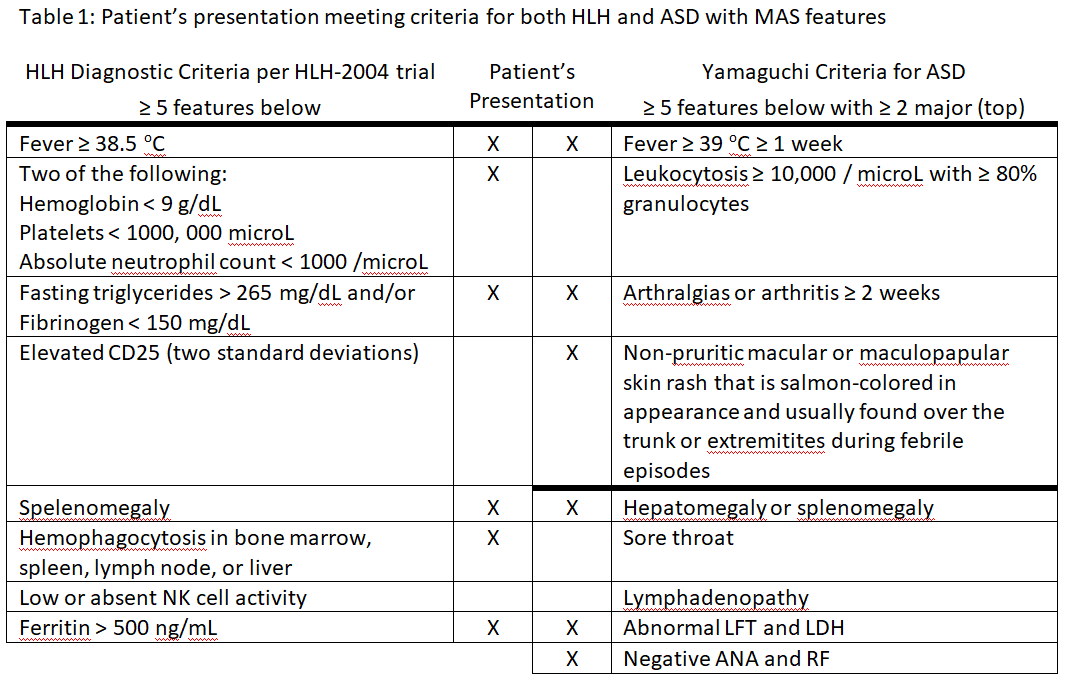
The patient underwent a punch biopsy of skin rash, which revealed perivascular lymphocytic infiltrate with neutrophils and a few histiocytes. The bone marrow biopsy revealed cellular bone marrow with trilineage hematopoiesis and rare hemophagocytosis, meeting 6 of 8 criteria for hemophagocytic lymphohistiocytosis (HLH), the etiology of which was further investigated.
Infectious studies including respiratory viral panel, acute hepatitis panel, QuantiFERON TB gold, Rocky Mountain spotted fever Ab, anti-Streptolysin O, EBV, CMV, Parvovirus, HHV-6, HSV, HIV, and blood cultures were negative.
Autoimmune serologic and immunologic studies revealed ESR at 11 (<28 mm/hr), CRP at 9.7 (<0.3 mg/dL), negative ANA, RF, anti-DNA, anti-SSA, anti-SSB, anti-scleroderma, ANCA, MPO/PR3, and cryoglobulin, and SPEP with no monoclonal gammopathy making Schnitzler’s syndrome unlikely. Adult Still’s disease (ASD) was suspected with Yamaguchi criteria. She was started on dexamethasone and discharged with improving clinical status and tapering steroid over the next few months confirming diagnosis of ASD with HLH.
Discussion: ASD is a rare autoinflammatory disorder characterized by intermittent fevers with salmon-colored rash, and arthritis/arthralgia. ASD is a diagnosis of exclusion and it can be associated with reactive HLH, which is also known as macrophage activation syndrome (MAS). MAS is an uncommon life-threatening complication characterized by pancytopenia, hypertriglyceridemia, normal or low haptoglobin, fibrinogen, and ESR despite high level of ferritin and CRP that occurs in about 12% of ASD patients. ASD should be considered in the differential presenting with these findings. Therapy is individualized, which can include: dexamethasone, etoposide, intrathecal methotrexate and hydrocortisone, and hematopoietic cell transplantation.
Conclusions: When ASD is associated with HLH, also known as MAS, patients tend to present with pancytopenia, very high triglyceride, normal or low haptoglobin and fibrinoen, and hemophagocytosis on bone marrow biopsy. MAS can be a life-threatening and it should be intervened early.