Background: At Thomas Jefferson University Hospital (TJUH) in Philadelphia, Pennsylvania, 4th year medical students can complete an elective in Perioperative and Consultative Medicine. The Farber Hospitalist Division is a unique Hospital Medicine Division in the Department of Neurosurgery that runs the medicine consult service and specializes in neurosurgical co-management at both TJUH Main Campus and Jefferson Hospital of Neuroscience (JHN).
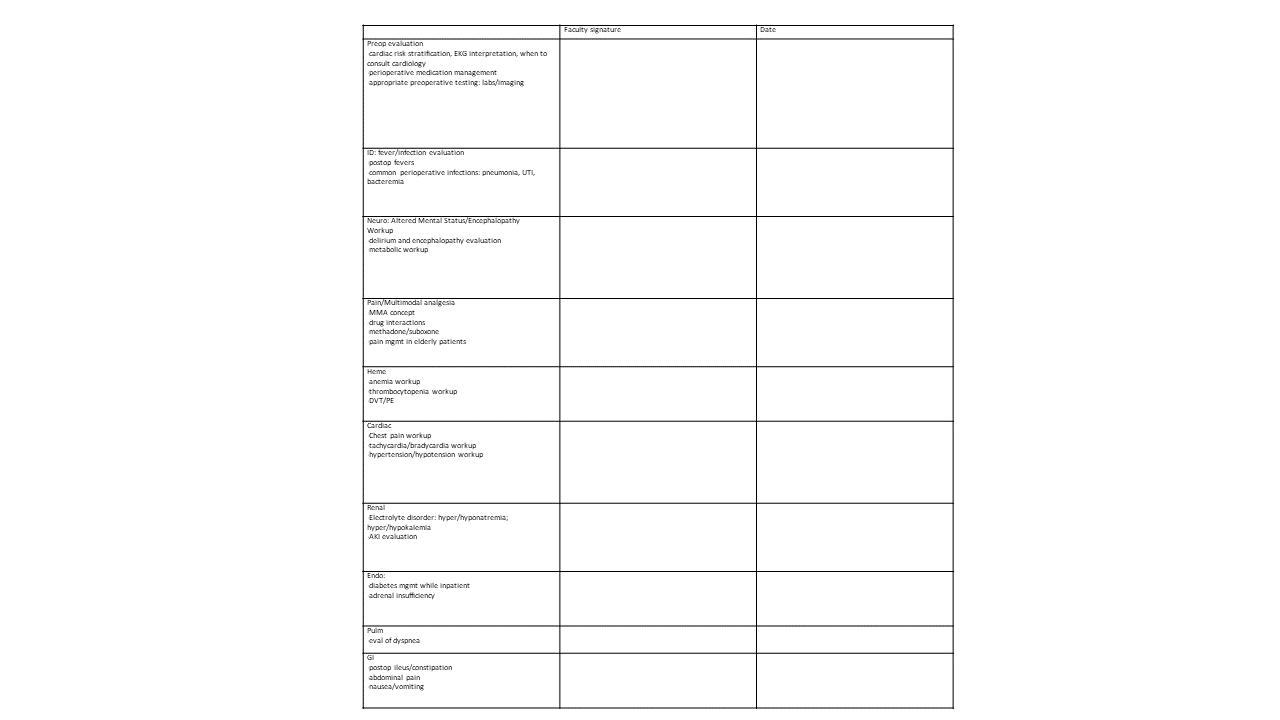
Purpose: The MED492 Elective was developed and implemented in September 2020. It is a 2-week, pass-fail rotation where fourth year medical students can be exposed to consult medicine and surgical co-management models and participate in the inpatient perioperative care of patients. As the field of perioperative medicine continues to grow, it is beneficial for medical students, especially those who are planning to pursue specialties in medicine, surgery and anesthesiology to have the opportunity to learn more about perioperative medicine and to hone their clinical skills with completing comprehensive preoperative evaluations and developing management strategies to medically optimize patients for surgery. Students can also consolidate their knowledge base and clinical skillset managing common medical problems that arise postoperatively such as postoperative pain, ileus, electrolyte abnormalities, fever, encephalopathy etc. A checklist of these high yield medical problems is provided at the start of the elective to encourage exposure and discussion of these topics. The checklist is also used as a tool to encourage teaching from the attending physicians and to standardize the student’s learning experience.
Description: Since the implementation of the elective, student feedback was collected and now analyzed to identify areas of strength and areas that need improvement. A total of 30 evaluations of former students were obtained and reviewed. Regarding the strengths of this elective, students expressed an appreciation for the abundant opportunities to complete and develop relative proficiency in performing preoperative assessments. They enjoyed working one-on-one with the attendings, and many commented that they valued the emphasis on teaching during this rotation. The checklist was also noted to be beneficial for reviewing key medical topics. Areas of improvement included the variability in the teaching quality between preceptors. Also, the number of new consults that come in and the exposure to different medical problems were variable depending on the day. Some students requested additional resources and reading material related to perioperative medicine. Some students wanted more customization of their elective experience and a more structured orientation at the beginning of the rotation.
Conclusions: Future steps to enhance this elective included setting up a standardized orientation at the beginning of the elective to outline student goals and expectations to allow for additional personalization of the elective. Landmark articles from the perioperative literature will be identified and provided as resources for the students and discussed during the elective. Teaching modules of high yield topics such as perioperative medication management, pain management and other topics will be created to further supplement the students’ learning. Ongoing student evaluations will be reviewed in the future for continued optimization of this elective in hopes that this elective can serve as a model for other institutions who may wish to start a similar program.