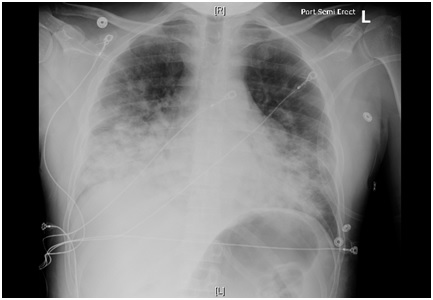
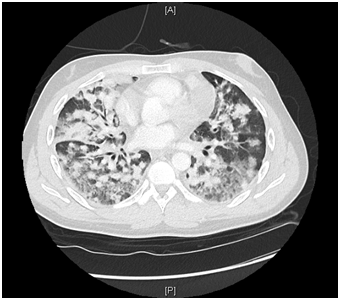
Case Presentation: A 35-year-old man was hospitalized with worsening shortness of breath, exercise intolerance and productive cough of two months duration. He also complained of blood in his sputum from 24 hours. He denied fever, chills, night sweats, or weight loss. Past history of asthma was noted. He had no history of tobacco, alcohol or drug use. He had a stable sexual relationship with a male partner and used a condom consistently.Patient was tachycardic with heart rate 108 bpm, mildly hypoxic with SpO2 of 93 % on ambient air. Physical exam was remarkable for generalized lymphadenopathy. CBC count showed a low neutrophil count 37% (43 – 75), lymphocytosis 53% (14 – 44 %), thrombocytopenia 57 X 103 / uL (149-390 103/uL). HIV 1/2 AB-AG combo was reactive for HIV 1 and HIV 2. Chest X Ray (Fig.1) showed patchy infiltrates and numerous pulmonary nodules in both lungs. CT chest with IV contrast (Fig.2) showed innumerable nodules throughout both lungs, irregular areas of ground glass attenuation along with mediastinal and retropectoral lymphadenopathy. Right inguinal lymph node excisional biopsy was positive for Kaposi Sarcoma.Patient was admitted with a diagnosis of Multifocal Pneumonia and a new diagnosis of AIDS (Acquired Immunodeficiency Syndrome). Bronchoscopy with (BAL) Bronchoalveolar Lavage was negative for any infection. Legionella and Streptococcal urine antigens were negative. Multispot HIV1/HIV2 confirmed HIV 1 positive. CD4 count 151 (359-1519/uL). Patient was started on antiretroviral therapy. Given the negative results of the comprehensive infectious work up and no significant improvement of lung imaging findings it was clinically and radiologically assumed that patient lung infiltrates and ground glass opacities were secondary to Kaposi Sarcoma involvement of the lungs, for which patient was started on Chemotherapy.
Discussion: Kaposi Sarcoma is an AIDS-Defining Illness; the clinical presentation of pulmonary KS is indistinguishable from other respiratory infections. Majority of patients present with dyspnea and cough, while a few can have fever, night sweats, hemoptysis, or chest pain [2]. Our patient fitted the typical clinical features; dyspnea, cough, hemoptysis. Primary Pulmonary involvement of Kaposi Sarcoma is estimated to happen only in about 15% of the cases [3]. It is more frequently seen associated with mucocutaneous manifestation as in our case. Often, respiratory symptoms in AIDS patients are attributed to top infectious pathogens such as Pneumocytis jirovecii, Histoplasma capsulatum or Mycobacterium tuberculosis. Bronchopulmonary involvement as an initial manifestation is a rare phenomenon [1]. Pulmonary KS can involve the lung parenchyma, airways, pleura, and/or intrathoracic lymph nodes. This case describes a young male patient who presented with pulmonary involvement of Kaposi Sarcoma at the time he was diagnosed with (AIDS) Acquired Immunodeficiency Syndrome
Conclusions: It is important to consider Pulmonary KS in a patient with HIV, subacute to chronic respiratory symptoms and negative infectious work up as the management of KS will require Chemotherapy in addition to ART (Antiretroviral Therapy) and will prevent complication of prolonged empiric antibiotic regimens. Lung biopsy which is the definite diagnosis tool for KS, was avoided in our patient due to risk of complications such as pneumothorax or hemorrhage and previously confirmed KS in lymph node excisional biopsy.