Background:
The Joint Commission's National Patient Safety Goals for 2008 and 2009 include numerous anticoagulation elements requiring hospitals to use approved protocols for the initiation and maintenance of anticoagulant therapy. Additionally, at our hospital, patients receiving warfarin on the Cardiac Surgery Service were noted to have an average length of stay (LOS) that was 2 days longer than patients not receiving warfarin. Previous published literature has demonstrated anticoagulation clinics staffed by pharmacists reduced bleeding episodes, thromboembolic events, hospitalizations and ER visits. Additionally, small studies of pharmacist‐guided dosing of warfarin for inpatients have shown a reduction in hospital LOS, supratherapeutic international normalized ratios (INRs), and posthospitalization bleeds and thromboembolic events.
Methods:
The study was designed as a pre/postintervention trial. Consecutive patients on the hospitalist and cardiac surgery services at the Hospital of the University of Pennsylvania who were prescribed warfarin from March 2007 through January 2008 were eligible. The AIM pharmacists collected preintervention data on all eligible patients, which served as the control cohort. The pharmacists then initiated written and verbal recommendations of warfarin doses on intervention patients based on a variety of clinical characteristics and dosing algorithms. Subsequently, they collected postintervention data on these patients. Outcomes collected included number of patients with INR > 4, median number of days on warfarin, median LOS, and 30‐day readmissions for reasons related to anticoagu‐lation. A chi‐square test was used for comparisons between groups for categorical variables, and a nonparametric rank‐sum test was used for median LOS and warfarin days.
Results:
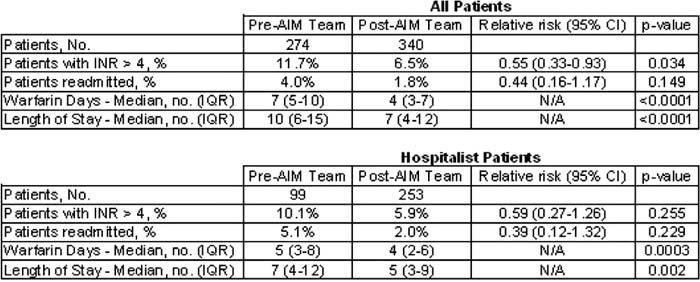
A total of 274 patients (99 hospitalists) were enrolled before the intervention, and 340 patients (253 hospitalists) were enrolled after the intervention. The unadjusted relative risk of an INR > 4 was significantly lower in the total postintervention cohort at 0.55 (95% Cl, 0.33–0.93; P = 0.034). The unadjusted relative risk of readmission after intervention was 0.44 (95% Cl, 0.15–1.27; P = 0.149), which was not statistically lower. The hospitalist subgroup showed similar relative risks for an INR > 4 (0.59, 95% Cl, 0.27– 1.36; P = 0.255) and readmission (0.39, 95% Cl, 0.12–1.32; P = 0.229), although these values were not statistically lower than prior to intervention. In the total cohort, the median LOS was reduced from 10 days (interquartile range 6–15) to 7 days (IQR 4–12, P < 0.0001), with an identical reduction of 3 days in the median number of warfarin days (P < 0.0001). The hospitalist cohort also showed significant reductions in median LOS (2 days, P = 0.002) and median warfarin days (1 day, P = 0.0003).
Conclusions:
The AIM team was able to reduce the frequency of supratherapeutic INRs as well as to reduce the median LOS through a reduction in the number of days patients spent in the hospital on warfarin.
Results
Author Disclosure:
T. Hecht, none; B. Birmingham, none; G. Gibson, none.