Background:
Numerous studies have shown that hospitalists in community settings reduce hospital costs primarily through reducing length of stay. Although some research in the academic setting indicates that hospitalist teaching attendings reduce mortality, little research has compared teaching services to nonteaching hospitalist care. We sought to compare patient outcomes for a nonresident hospitalist service versus a teaching service.
Methods:
All general medicine patients at our academic medical center are admitted either to a hospitalist service with no residents or to a teaching service. We sampled 883 charts from an ongoing retrospective chart review of all general medicine patients admitted between January 1, 2008, and October 31, 2008, choosing 239 sequential admissions in January, 305 in April, and 339 in August to reflect 3 different points in the academic year. Each patient was classified as “hospitalist service” or “teaching service” based on whether a hospitalist or resident admitted the patient. We assessed the following outcomes: length of stay, ICU days during hospitali‐zation, repeat ED visit or readmission within 30 days of discharge, time to repeat ED visit or readmission after discharge, poor outcome within the first 24 hours (defined as ICU transfer, cardiac arrest, or death), and hospital charges.
Results:
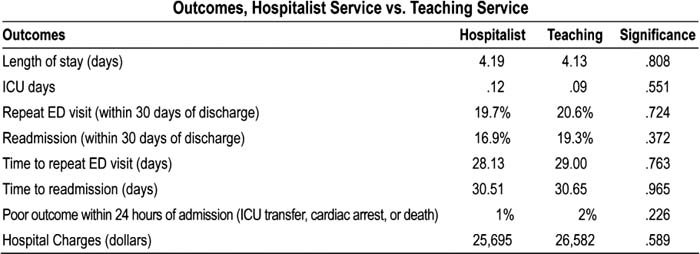
Of 883 charts examined, 96% (402 hospitalist service, 446 teaching service) had complete data available for analysis. Baseline characteristics were similar between services in terms of age and sex, with a trend toward increased case mix (complexity) on the teaching service (P = 0.09). Patients admitted to the hospitalist service compared with to the teaching service had the following outcomes: length of stay, 4.19 versus 4.13 days; ICU days, 0.12 versus 0.09 days; repeat ED visit within 30 days, 19.7% versus 20.6%; readmission within 30 days, 16.9% versus 19.3%; time to repeat ED visit, 28 versus 29 days; time to readmission, 31 versus 32 days; poor outcome within the first 24 hours, 1 % versus 2%; and hospital charges, $25,695 versus $26,582. None of these outcomes were significantly different (all P > 0.20). There was also no significant difference in patient outcomes after adjustment for case mix (all P > 0.40).
Conclusions:
In a sample of general medicine inpatients during a 10‐month period at 1 academic center, there were no significant differences in outcomes for patients admitted to a hospitalist service versus those admitted to a teaching service. We believe the use of hospitalists as almost half the teaching attendings may help to account for the similar performances. Further research is needed to determine whether the advantages conferred by hospitalists on inpatient care relate primarily to their expertise, or whether their presence and accessibility within the hospital also play a significant role.
Author Disclosure:
R. Khanna, none; K. Wachsberg, none; A. Marouni, none; L. Lindquist, none; J. Feinglass, none: D. Wayne, none; M. Williams, none.