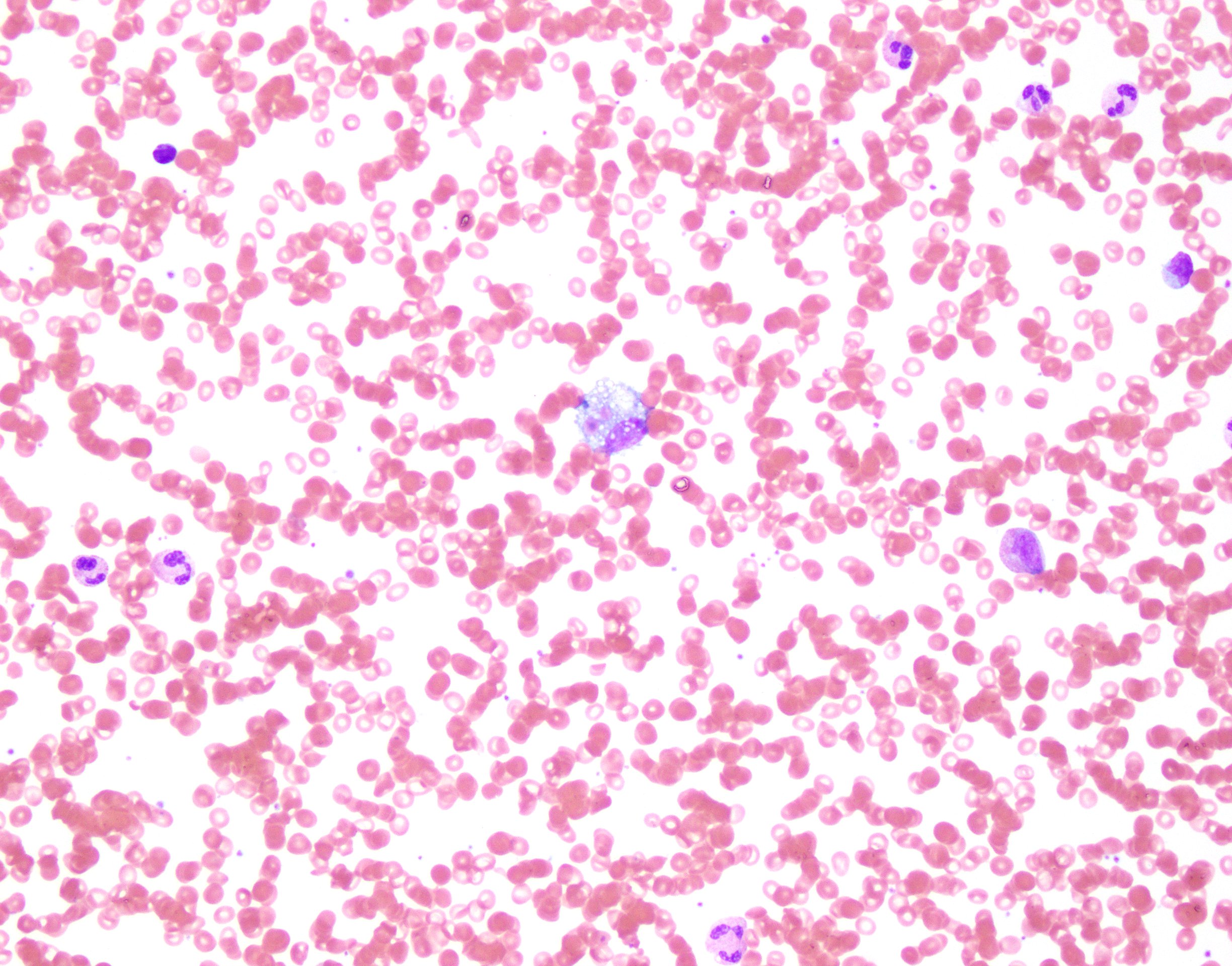
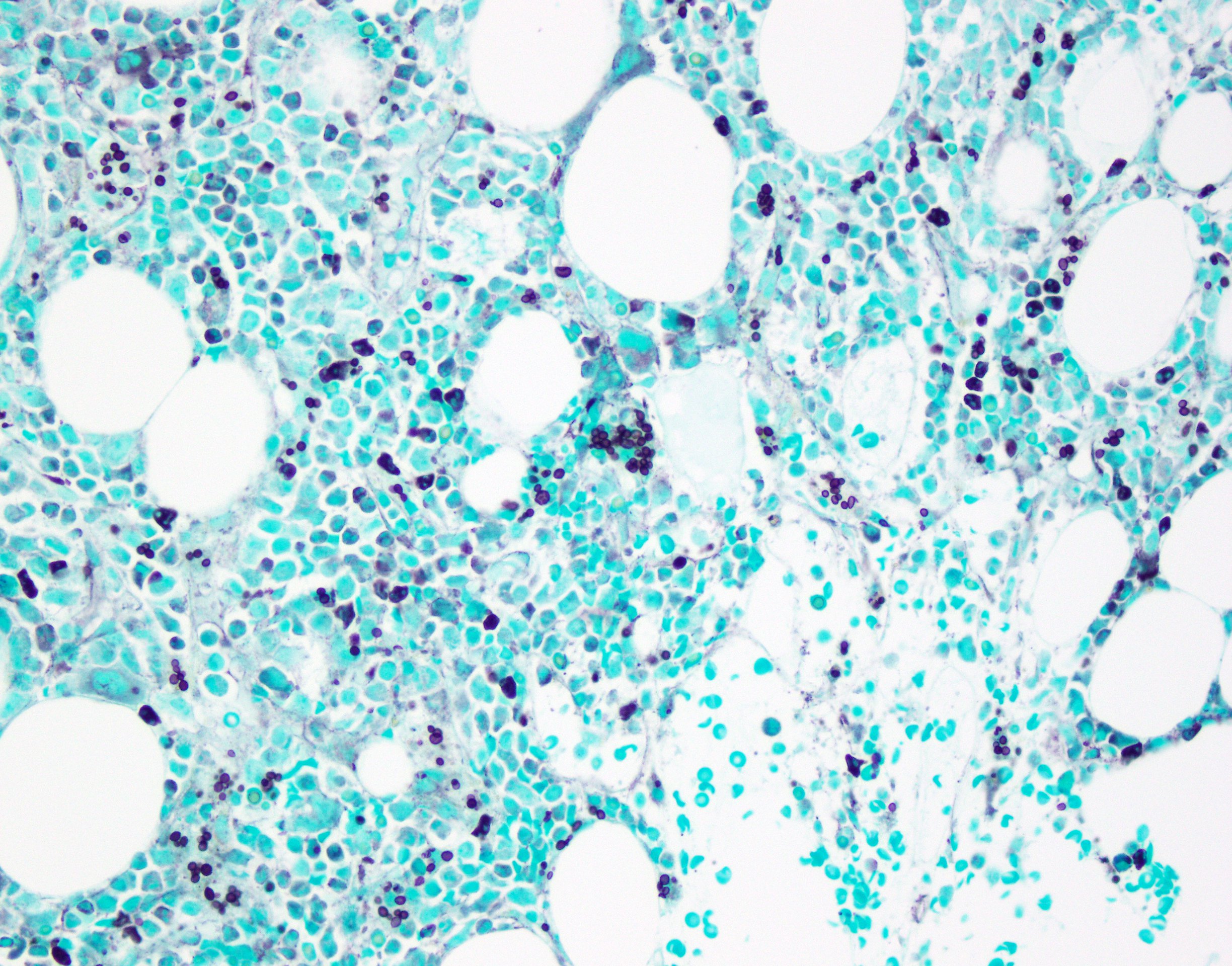
Case Presentation: A 44 year-old man who resides in Alexandria, LA presented via air ambulance from Honduras with three weeks of fever, night sweats, and right upper quadrant abdominal pain. He had associated nausea, vomiting, diarrhea, and headache. Exam was notable for fever and hepatomegaly. Serum studies revealed a creatinine of 6 mg/dL, elevated AST, ALT, alkaline phosphatase and GGT, as well as a microcytic anemia and thrombocytopenia. A 4th generation HIV test returned positive. CD4+ count was 7/mm3. HIV viral load was >10 million copies/mL. Acute viral hepatitis serologies and T-SPOT were negative. Lumbar puncture was performed with unremarkable CSF studies and a negative CSF cryptococcal antigen. Abdominal CT displayed only splenomegaly. Ferritin was >15,000 ng/mL and fasting triglycerides were elevated. A urine histoplasma antigen returned positive. Bone marrow biopsy revealed no malignancy but showed hemophagocytic histiocytes and numerous intracellular yeast forms compatible with Histoplasma spp. Renal biopsy exhibited budding yeast in the interstitium with associated acute and chronic inflammation and tubuloepithelial injury. Serum soluble IL-2 was within normal limits and NK cell function was borderline elevated. Routine and AFB blood cultures and CSF cultures were sterile. In addition to starting abacavir/lamivudine and dolutegravir, the patient was treated with liposomal amphotericin B induction for two weeks before transitioning to oral itraconazole. Three months after discharge he remains in care with evidence of renal recovery.
Discussion: Histoplasma capsulatum is an endemic fungus that can cause disease in immunocompetent and immunocompromised hosts. Patients with cellular immune dysfunction are at risk for hematogenous spread of primary pulmonary infection. This patient meets criteria for progressive disseminated histoplasmosis by both laboratory and pathologic evidence. This disease entity is fatal without treatment. Liposomal amphotericin B induction with itraconazole maintenance is the preferred therapy and highly effective. Though renal dysfunction is common with disseminated histoplasmosis, amphotericin B therapy is still recommended given its efficacy weighted against the poor prognosis of this disease. The criteria for confirmed hemophagocytic lymphohistiocytosis (HLH) were also met. This hyperactive immune response has been associated with disseminated intracellular infections such as histoplasmosis, especially among AIDS patients. The treatment of secondary HLH is directed at the underlying cause. The role for chemotherapy and immunosuppression in histoplasmosis-associated HLH is currently unknown as is the best timing for antiretroviral initiation in those cases associated with HIV infection.
Conclusions: Recognition of the underlying cause in secondary HLH is critical to prevent further morbidity and mortality in patients. When disseminated histoplasmosis is suspected, hospitalists should begin treatment immediately to improve outcomes.