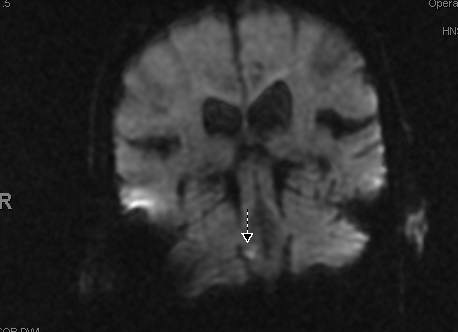
Case Presentation: 84-year-old male with past medical history of Hypertension, lacunar thalamic infarct presented for evaluation of dizziness which started 30 minutes prior to ED arrival. His vitals were remarkable for elevated blood pressure 172/97. He was noted to be ataxic, otherwise, no neurological deficits noted on initial physical exam. His labs were remarkable for low potassium of 2.8 mMol/L. ECG was remarkable for rate-controlled Atrial Fibrillation with RBBB. CT head was negative for acute infarction or bleed. 7 hours after initial presentation, the patient was noted to have a slight right-sided facial droop. Stat MRI brain, MRA brain & neck, CTA head & neck were obtained. MRI showed an old right thalamic lacunar infarct but was unremarkable for any acute infarction. MRA showed a completely occluded LICA. CTA re-demonstrated completely occluded LICA and also showed a focal occlusion of right vertebral artery distal to the origin of PICA. LICA occlusion was deemed to be chronic. The patient continued to have dizziness, right facial droop and ataxia next morning. The clinical suspicion for posterior circulation CVA was high and therefore MRI brain with coronal sections DWI was obtained which revealed a focal area of acute to subacute ischemic infarction involving right posterior medulla confirming the underlying etiology of his symptoms. Heparin drip was started given the newly diagnosed atrial fibrillation and was subsequently transitioned to coumadin. High dose statin therapy was initiated and aspirin which he was already on at home was continued. His symptoms improved over the course of his hospitalization. He was discharged to inpatient rehab.
Discussion: About one-fifth of ischemic cerebrovascular events affect posterior circulation or the vertebrobasilar system with the resultant lesions being in the thalamus, cerebral peduncle, brainstem or parts of occipital, parietal or temporal lobes. The patients can present with a multitude of signs and symptoms with the most common ones being dizziness, dysarthria, nausea, limb weakness, ataxia, and nystagmus. MRI with DWI is a highly sensitive study for early detection of ischemic strokes, however, sensitivity is not 100% resulting in a few false negatives. The likelihood of false negatives is higher in posterior circulation strokes. In these cases, obtaining coronal sections DWI in addition to standard axial sequences on MRI can clinch the diagnosis. Our patient had clinical presentation highly suggestive of a posterior circulation event with negative standard axial MRI DWI but coronal DWI sequences confirmed a medullary stroke.
Conclusions: Hospitalists frequently encounter patients with symptoms like dizziness, ataxia, vertigo which can although suggest a vertebrobasilar insufficiency but at the same time are nonspecific in nature and can have other underlying etiologies. A negative standard axial MRI with DWI in these cases can be reassuring but at the same time misleading if the study is a false negative. If the clinical suspicion for such an event is high, coronal DWI should be obtained in addition to standard axial MRI with DWI.