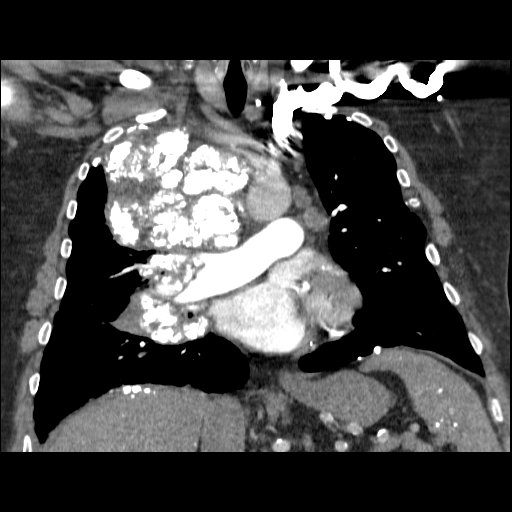
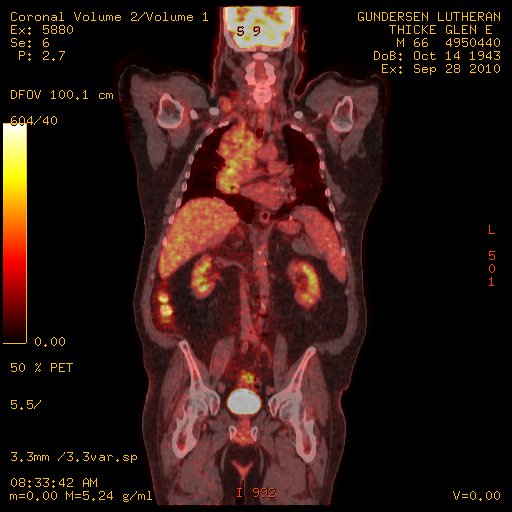
Case Presentation: A 65 year-old man with a past medical history of CAD s/p CABG, ischemic cardiomyopathy with EF 35%, bicuspid aortic valve stenosis s/p aortic valve replacement, and asbestosis presented to the ER for evaluation of anterior neck swelling, dyspnea on exertion, dysphagia, and a 30 lb unintentional weight loss over 5 months. On initial evaluation, his vitals were significant for HR 95, BP 133/78, RR 25, O2 % saturation 93 on 2L NC, and Temperature 37.5 F. Physical examination revealed anterior neck swelling with facial plethora, respiratory distress, systolic ejection murmur with elevated JVP, and bilateral crackles on auscultation. Initial laboratory workup was largely unremarkable. Electrocardiogram revealed a normal sinus rhythm with chronic right bundle branch block. Chest X-ray revealed a large calcified mass along the right mediastinum with associated calcified right supraclavicular nodes and bilaterally calcified pleural plaques (known asbestosis). A CT chest with IV contrast revealed partially calcified masses and adenopathy involving the right neck, right mediastinum, and right hilum and SVC narrowing. He was admitted to the hospital for further evaluation. Due to concern for malignancy, a PET-CT was obtained and showed extensive FDG avid mediastinal and hilar adenopathy, concerning for lymphoma vs amyloidosis. A cardiac MRI revealed signs of ischemic cardiomyopathy but was not indicative of an infiltrative disease. A supraclavicular lymph node biopsy showed extensive AL amyloid deposition while bone marrow biopsy and fat pad aspirate were negative for systemic involvement of amyloidosis. The patient was finally diagnosed with tumoral amyloidosis and was treated with corticosteroids and radiation.
Discussion: Amyloidosis is characterized by extracellular deposition of fibrillary proteinaceous material resulting in tissue damage. Amyloidosis can be systemic, organ limited, or localized. Amyloidomas (tumoral amyloidosis) are localized tumors of amyloid deposits and diagnosis hinges on identifying these localized masses of amyloid in the absence of systemic amyloidosis. Amyloidomas are the least common form of amyloidosis but have been reported in the brain, lung, GI tract, head/neck region, and soft tissues. Based on the location of these tumors, patients present in various ways. Importantly, patient’s can develop compressive symptoms of vital organs which requires hospitalization and inpatient care. As exemplified by our patient, his mediastinal mass led to compression of his SVC and right lung leading to a partial SVC syndrome with facial plethora, respiratory difficulty, and dysphagia. Treatment of amyloidomas can be multimodal but typically involves surgical resection. Depending on the type of amyloid, patients can eventually develop systemic amyloid or a lymphoplasmacellular malignancy. Due to the complex location and vascular abutment of this patient’s amyloidoma, he was treated with corticosteroids and radiation. He has been followed routinely every 6 months.
Conclusions: Amyloidomas, the least common form of amyloidosis, are defined as localized tumor like amyloid deposits in the absence of systemic disease. Tissue biopsy is key for diagnosis. Based on the location of the tumor, they can exhibit compressive symptoms requiring hospital admission and management. Treatment typically involves local resection but radiation can be considered. Routine monitoring is required to rule out progression to systemic amyloid or lymphoplasmacellular malignancy.