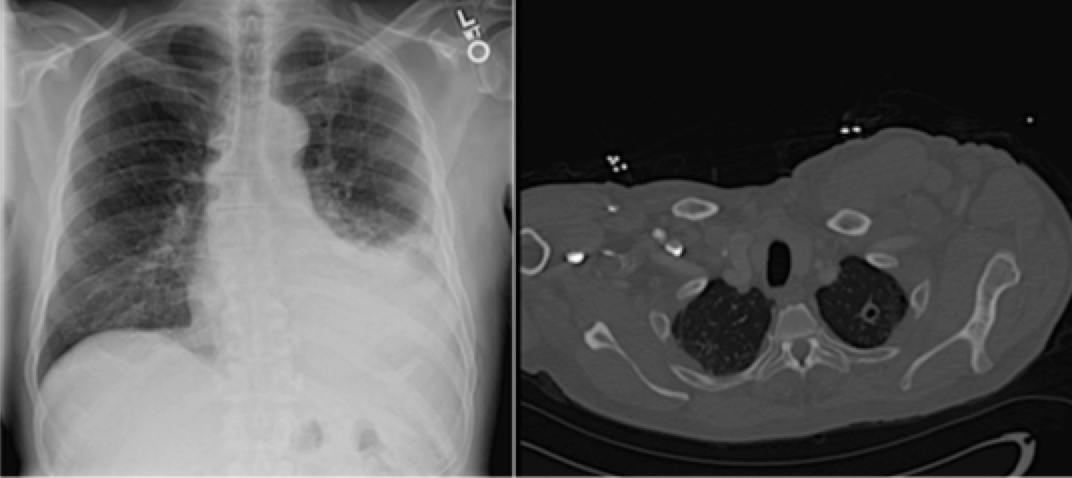
Case Presentation: A 61-year-old African American male with history of recent atopic dermatitis treated with topical corticosteroids presented with 4 days of fevers, night sweats and worsening exertional dyspnea. On admission, he was febrile with decreased left lower lobe breath sounds. CT showed a moderate left-sided pleural effusion and left upper lobe cavitary lesion. The differential included both infectious and malignant etiology with infection being higher on the differential due to the relative rapid onset of the patient’s symptoms. Two sputum samples returned negative for acid fast bacilli (AFB), fungal and bacterial cultures. A third sputum was not collected due to absent productive cough. Over the hospital course, the patient underwent three thoracenteses, which demonstrated a lymphocytic exudative effusion. Pleural studies were negative for AFB and cytology was negative for malignancy. Pleural adenosine deaminase (ADA) levels were mildly elevated, rising on serial thoracenteses from 29.7 to 40.9. Given persistent fevers, a positive quantiferon, a cavitary lung lesion and a lymphocytic pleural effusion, the patient was started on RIPE therapy for treatment of presumptive tuberculosis (TB) with symptom improvement. Subsequent pleural biopsy demonstrated granulomatous changes. The patient’s pleural biopsy and fluid grew TB five weeks after initial presentation, confirming a diagnosis of extrapulmonary pleural TB.
Discussion: TB is a major global health concern with increasing atypical presentations. Extrapulmonary tuberculosis (EPTB) occurs in about 25% of TB patients, and if left untreated can lead to significant morbidity and mortality. It is necessary for clinicians to be aware of the various manifestations of pulmonary TB and EPTB. Our patient demonstrates the value of keeping a wide differential and not relying on one lab finding when considering the diagnosis of TB. Despite negative AFB sputum and pleural fluid with only mildly elevated pleural ADA levels on initial evaluation, a diagnosis of EPTB was confirmed. Given his typical presentation of a cavitary lung lesion and exudative lymphocytic pleural effusion, further workup with pleural biopsy was pursued and showed granulomatous changes typical of pleural TB. The patient may have become immunocompromised with recent topical corticosteroid use for treatment of atopic dermatitis contributing to a rapid clinical deterioration.
Conclusions: This case illustrates the importance for hospitalists to be aware of atypical presentations of TB in which early detection can promote better patient outcomes. Patients with AFB smear-negative TB can rapidly progress, especially if immunocompromised. The significant risk of increasing mortality justifies the advantage of early detection and treatment. As AFB sputum and ADA levels may not always be indicative of TB, further workup is necessary in cases where suspicion remains high despite atypical lab findings.