Background: The occurrence of adverse events due to unsafe health care is thought to be one of the 10 leading causes of death and disability in the world. The harm can be caused by a range of adverse events, with nearly 50% of them preventable. Broad adoption of electronic health records (EHR) should ideally harness the power of technology to help reduce medical errors. We present a novel tool for addressing opportunities to improve patient safety and prevent adverse events, which we refer to as safety gaps. Our tool integrates safety gap identification, alerts, and appropriate actions into a single interface that is embedded within clinicians’ typical workflow. The tool uses existing capabilities within Epic, the most widely used EHR nationwide, to facilitate addressing patient safety issues within our institution.
Purpose: Given the significant role of the EHR in provider workflow, we aimed to leverage the data, functionality, and display of Epic, our institution’s EHR, to identify and address safety gaps in patient care. Several key patient safety issues were selected based on published literature on safe inpatient care. We created a tool to (1) alert providers to these safety issues for each patient, (2) easily address safety gaps with as few clicks as possible, (3) display the information on the commonly used patient list view, and (4) communicate the status of safety issues to other providers. The tool is meant to impact safety outcomes while making providers’ workflows more efficient.
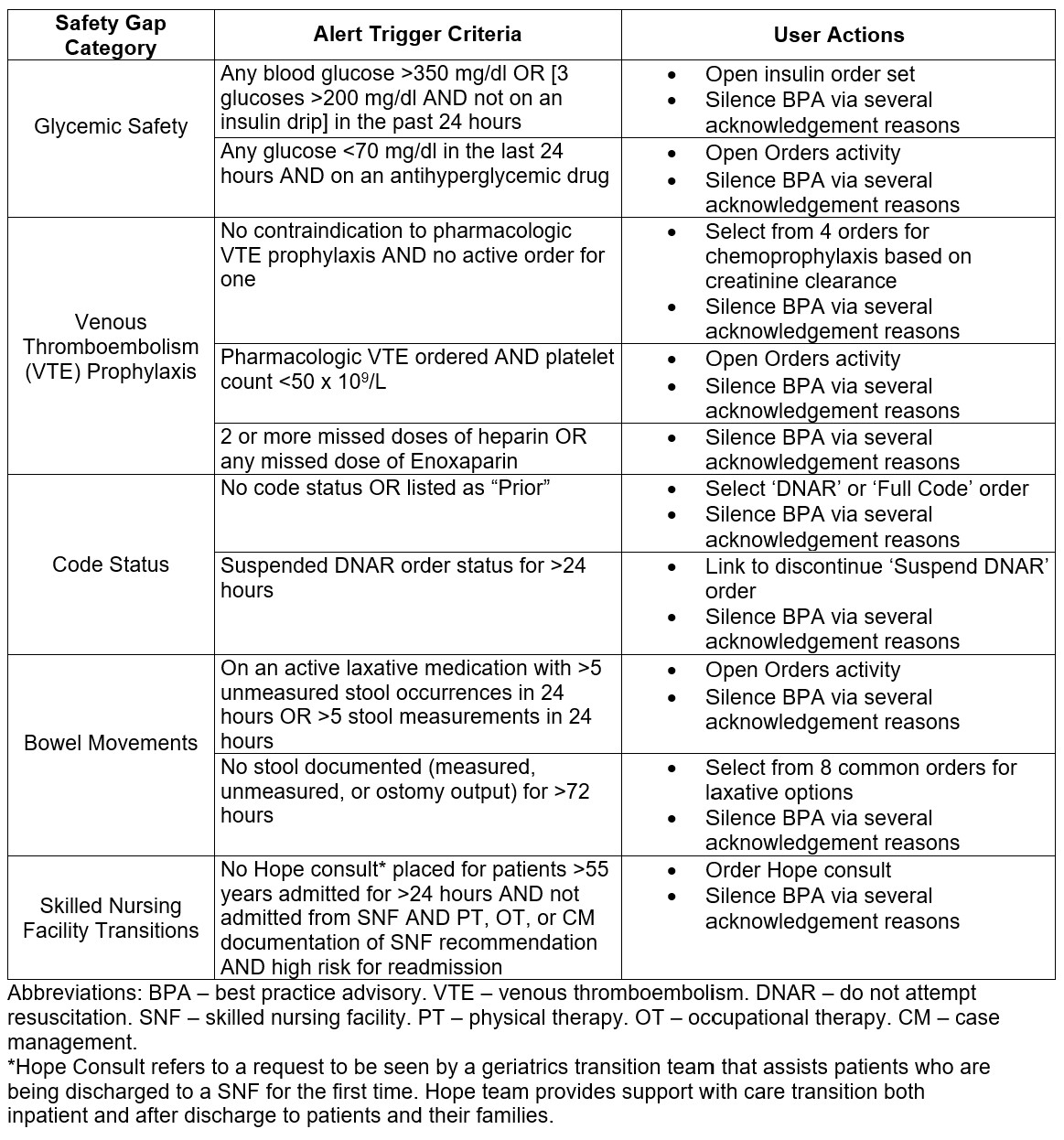
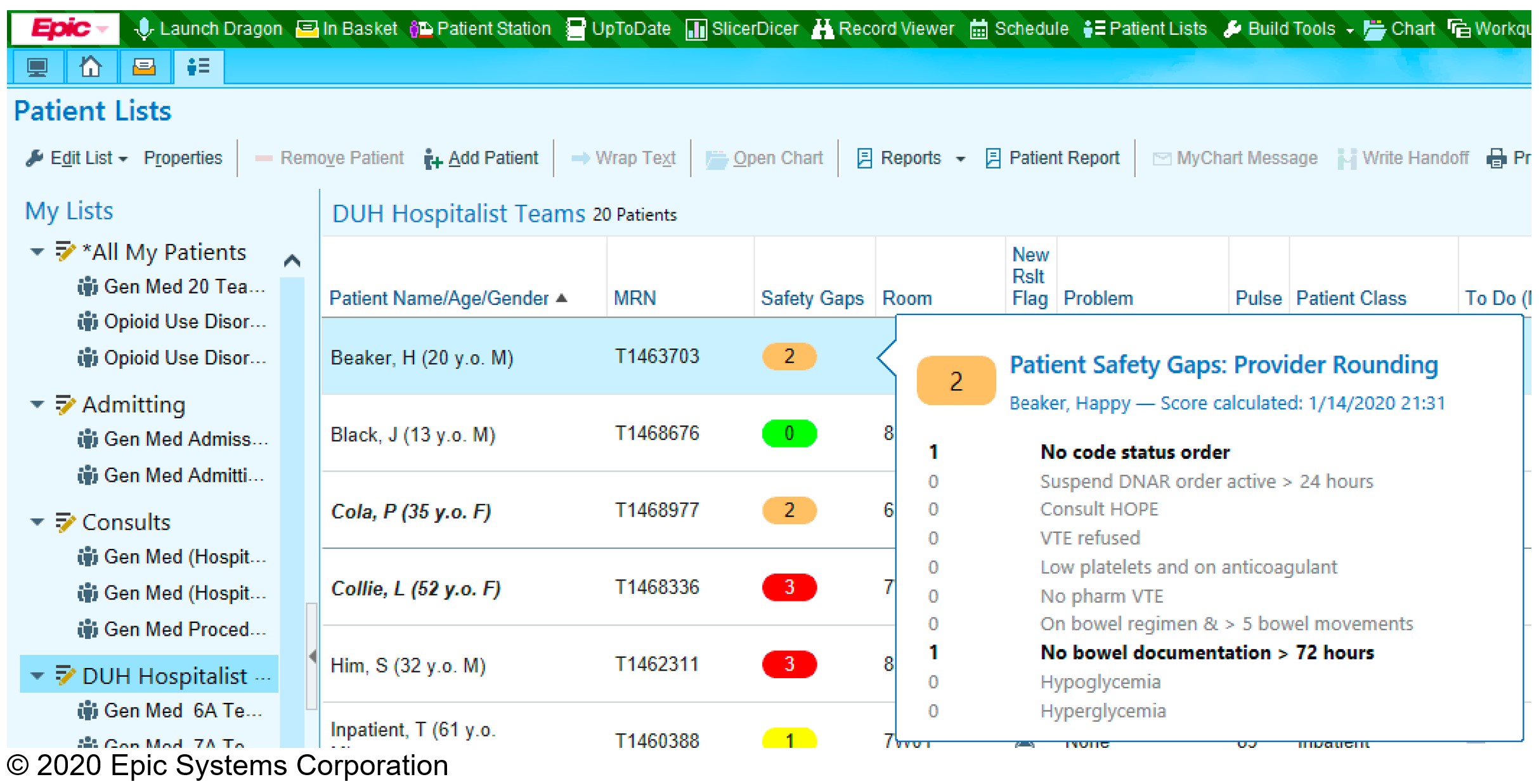
Description: A safety gap tool was developed to address five categories and ten specific key safety gaps determined by the Duke University Hospital Medicine team (Table 1). The tool regularly retrieves data to identify preprogrammed gaps, deriving data from Epic including demographics, orders, laboratory values, flowsheets, and medication administration records. If a safety gap is identified, the provider receives a passive alert via their patient list encouraging them to act on the safety gap or acknowledge the reason for not acting. The patient list column in Epic allows the user to hover to discover more information and incorporates a green/yellow/orange/red color scheme to gamify to the tool, ideally driving providers to achieve an all-green column without disrupting efficiency (Figure 1).
Conclusions: A safety gap tool was successfully built within an academic medical center to address key patient safety issues. Early results demonstrated that the most prevalent safety gaps in our patient population were lack of venous thromboembolism prophylaxis (40.4% of all alerts), constipation (19.3%), and lack of a code status (18.4%). Of patients with at least one alert, the average burden was 2.1 alerts per patient per day. Formal usability testing showed widespread acceptance and positive regard for the tool without significant concern for alert burden given the passive nature of the tool. The tool’s strengths are its integration within the EHR, its ease of use, and its scalability as new safety gaps are identified in our or other institutions. Further work is required to expand to all inpatient services and increase utilization. This work can be applied to other large health systems, particularly those using Epic, to identify and address their organization’s major safety gaps, leading in reduction of patient safety issues and preventable errors.