Background: “Time is brain” is a trope from the neurologist Camilo Gomez that emphasizes the importance of early treatment to improve the neurological prognosis of ischemic stroke patients. Given the short therapeutic window of evidence-based therapies such as thrombolysis and endovascular treatment, it is important to diagnose ischemic stroke from the numerous possible diagnoses accurately and without delay. Nevertheless, few studies have investigated the prevalence of missed opportunities for the effective treatments of ischemic stroke due to delayed diagnosis. Therefore, we investigated the prevalence of missed ischemic stroke diagnosis at initial contact, the risk factors associated with delayed diagnosis, and the prevalence of potentially treatable patients without a delayed diagnosis in a Japanese hospital.
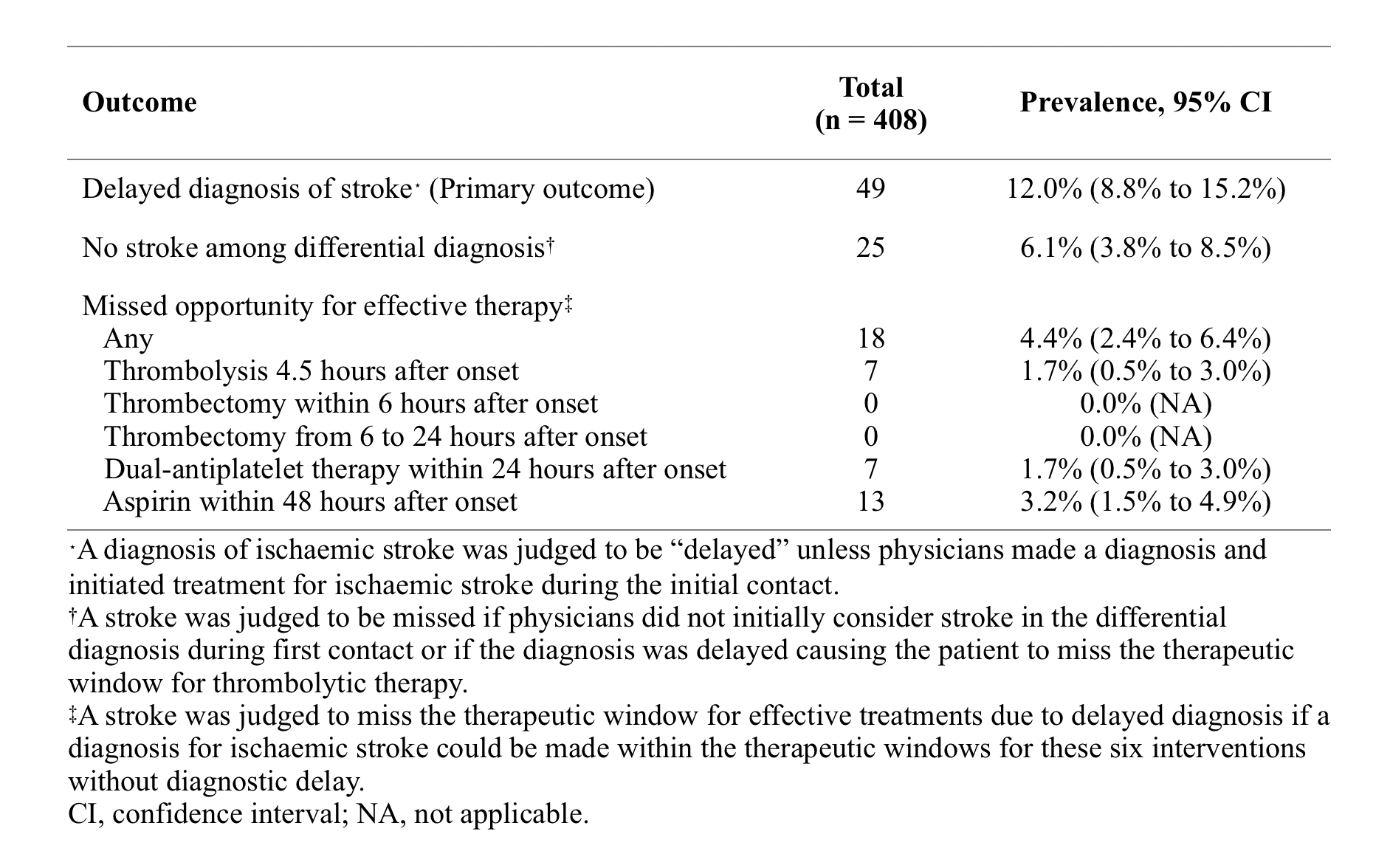
Methods: A retrospective (from April 2017 to July 2019) and prospective (from August 2019 to October 2020) observational study were conducted by reviewing electronic medical records. A total of 408 consecutive patients hospitalized due to acute ischemic stroke in our hospital were included. We included only magnetic resonance imaging-proven ischemic stroke patients. Patients who were suspected of having or diagnosed with ischemic stroke at other hospitals were excluded. The primary outcome was the delayed diagnosis of ischemic stroke at the initial contact. A stroke diagnosis was deemed “delayed” unless physicians made a diagnosis of and initiated treatment for ischemic stroke during the initial contact. The secondary outcome was ischemic stroke with a missed therapeutic window for effective treatment (such as thrombolysis, endovascular treatment, and antiplatelet therapy) due to delayed diagnosis.
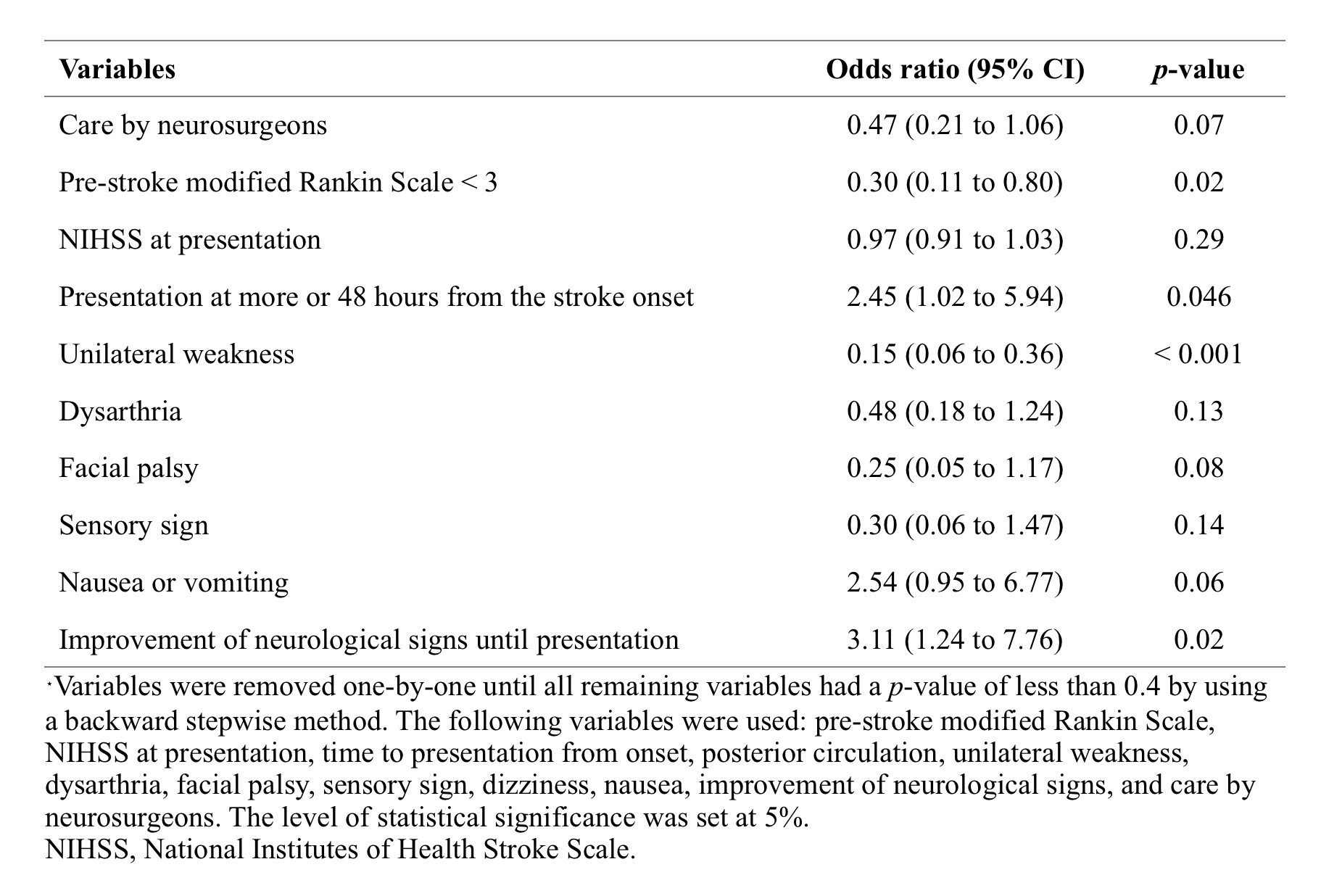
Results: Of all included patients, the median age was 78 years old, 170 (41.7%) were women, 100 (24.5%) had a history of stroke, and the median pre-stroke modified Rankin Scale (mRS) score was 0. The median time to presentation from the time the patient was last known to be well was nine hours, and the median NIHSS score at presentation was 4. A diagnosis of stroke was deemed delayed in 49 (12.0%) patients. The most common initial diagnosis at first contact in the ischemic stroke patients with delayed diagnoses was epilepsy (n = 8), followed by dizziness (n = 6) and head trauma or concussion (n = 4). Of the 49 delayed diagnosis patients, 16 (33%) missed the opportunity to receive effective treatment at the initial visit. However, no stroke cases missed thrombectomy opportunities. In the multivariable analysis, presentation at 48 hours or more from the stroke onset (OR 2.45, 95%CI 1.02 to 5.94) and improvement of neurological symptoms until presentation (OR 3.11, 95%CI 1.24 to 7.76) were independently associated with an increased risk of delayed diagnosis of ischemic stroke. Conversely, hemiplegia (OR 0.15, 95%CI 0.06 to 0.36) and a pre-stroke mRS score less than 3 points (OR 0.30, 95%CI 0.11 to 0.80) were independently associated with a decreased risk of delayed diagnosis of ischemic stroke.
Conclusions: Even in the modern era, one in every eight ischemic stroke cases was missed at the initial visit, and one-third of missed strokes might be candidates for effective treatment without diagnostic delay. Further efforts to avoid missing the therapeutic window for effective interventions for ischemic stroke due to delayed diagnosis are required, particularly for patients with disabilities or whose neurological signs improve before presentation.