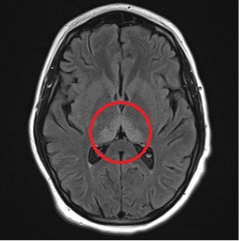
Case Presentation: A 16 year old boy with obesity presented for dehydration in the setting of three months of abdominal pain, nausea, and non-bloody, non-bilious emesis. Outpatient work-up had been unrevealing. He also endorsed cannabis use and vaping. He had lost 70 pounds during this time. New symptoms in the days prior to admission included dizziness and double vision.On admission, his physical exam was significant for horizontal nystagmus. An ophthalmology exam was normal. A brain MRI was unremarkable. The initial differential for his GI symptoms included cannabis hyperemesis syndrome, cyclic vomiting, and gastroparesis. Neurology was consulted for nystagmus; labrynthitis, vestibular neuritis, and benign paroxysmal positional vertigo were all considered. Despite intravenous fluids and antiemetics, the patient had ongoing nausea and vomiting. He developed vertical nystagmus on hospital day 4. There was a discussion with neuro-ophthalmology who suspected ingestion as the cause of his ocular symptoms. On hospital day 7, the patient developed confusion and slurred speech. This progressed to include visual hallucinations, agitation, and urinary retention over the next 24 hours. The differential was expanded to consider seizures, encephalitis, vitamin deficiency, and drug reaction. Electroencephalogram was negative. Due to ongoing agitation and hallucinations, the patient was transferred to the PICU. An extensive cerebrospinal fluid evaluation ultimately returned negative. A repeat brain MRI was obtained which showed new increased T2/FLAIR signal hyperintensity in the bilateral thalami, mamillary bodies, and periaqueductal gray matter, consistent with Wernicke’s encephalopathy.The patient was started on high dose intravenous thiamine with improvement in his mental status and resolution of hallucinations. His thiamine level did ultimately return low.
Discussion: Wernicke’s encephalopathy is classically associated with alcoholism but has been documented in myriad conditions. Autopsy studies indicate that it is underdiagnosed.(1) Case reports describe Wernicke’s in pediatric patients with malignancy, eating disorders, intestinal surgery, and others. When suspected, it is important to treat empirically as thiamine levels can take several days to return. Symptoms can worsen if patients are given dextrose without concurrent thiamine repletion. Wernicke’s is reversible but exists on a spectrum depending on the duration of deficiency and permanent cognitive impairment can be seen (Korsakoff syndrome).In this case, the diagnosis was not made until hospital day 9. This delay is likely attributable to several factors. Wernicke’s is frequently considered an adult diagnosis and may not be on the differential of pediatric providers. Even if it had been considered, the initial normal MRI may have prematurely removed it from providers’ differential. Then despite a significant weight loss, this patient was still obese which may not have triggered providers to consider him malnourished.
Conclusions: This case highlights the importance of maintaining a high index of suspicion for conditions less commonly seen in pediatrics, particularly when symptoms are progressing. Wernicke’s can be seen in malnourishment for any reason, which can be present despite obesity. It is important to avoid premature closure and anchoring bias on initial suspicion, in this case ingestion in the setting of drug use. Nystagmus should trigger a broad differential especially when accompanied by other neurologic symptoms.