Background: Patients with substance use disorders (SUDs) are at high risk for blood borne viruses (BBV) and sexually transmitted infections (STIs).1 Syphilis infections, in particular, have dramatically increased over the past decade. More patients with syphilis infections are reporting injection drug use.2 Hospitalization is considered a “reachable moment” for this vulnerable patient population.3 Yet, screening rates remain low.4
Purpose: We developed an electronic medical record best-practice advisory (BPA) to encourage hospital providers to screen patients with SUDs for STIs (Figure 1). We examined inpatient screening tests for HIV, viral hepatitis and syphilis in the pre-intervention period (December 2023 and January 2024) to post-intervention period (February 2024 through August 2024).
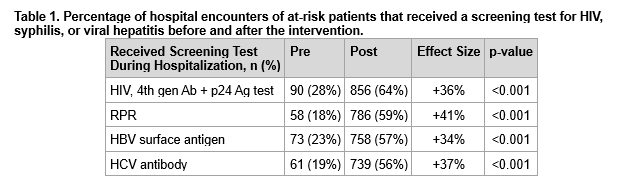
Description: The BPA was designed to trigger on hospitalized patients at Barnes-Jewish Hospital with an ICD-10 diagnosis of F11.x, F14.x, F15.x and F19.x and if they did not have a fourth-generation HIV test, hepatitis B surface antigen, or hepatitis C antibody within the previous 12 months.After implementation of the BPA, the proportion of patient-encounters that received testing for HIV, viral hepatitis, and syphilis increased (Table 1). In the pre-intervention period, 90 (28%) were tested for HIV, 58 (18%) for syphilis, 73 (23%) for hepatitis B, and 61 (19%) for hepatitis C. In the post-intervention period, 856 (64%, p-value < 0.001) were tested for HIV, 786 (59%, p-value < 0.001) for syphilis, 758 (57%, p-value < 0.001) for hepatitis B, and 739 (56%, p-value < 0.001) for hepatitis C. In the post-intervention period, a total of 3 (0.35%) patient-encounters had a reactive 4th generation HIV test, all of which were determined to be false positives. 35 (4.45%) patient-encounters had a reactive RPR, of which 18 (51%) were new diagnoses. 8 (1.06%) patient-encounters had a reactive hepatitis B surface antigen, of which 4 (50%) were new diagnoses. 739 (56%) patient-encounters were HCV Ab positive, with an RNA positivity rate of 37%.
Conclusions: An electronic medical record BPA was able to increase screening for HIV, syphilis, and viral hepatitis among hospitalized patients with SUDs.