Background: Sepsis, severe sepsis, and septic shock combined, are estimated to affect between 650,000 and 750,000 Americans annually, and has an associated mortality rate between 20 to 50%. Early identification of patients with sepsis is critical, as treatment delays are associated with significant increases in mortality. The electronic health record (EHR) contains near-real-time physiologic parameters, lab values, orders, and medical history and thus is an increasingly useful platform for clinical decision support. Efforts to utilize EHR data for sepsis alerting have so far had mixed results. In this quality improvement effort, we randomly assigned patients with clinical parameters suggesting severe sepsis to eihter send their providers a severe sepsis alert or to usual-care.
Methods:
Population: 1169 consecutive adults age 18 or older admitted to inpatient wards (no intensive-care units) at Stanford Hospital between November 2014 and March 2015.
Intervention: Patients randomized to the experimental arm generated a text-page to a critical-care nurse and an internal medicine resident in the case of medical patients, and to only a critical-care nurse in the case of surgical patients.
Comparison: Patients randomized to the usual care arm did not generate the alert but received all usual clinical care.
Outcome: Primary Outcome: Percentage of patients who received the complete sepsis bundle: broad-spectrum antibiotics, intravenous fluids, serum lactate, and blood cultures within 3 hours of alert. Secondary Outcomes: time between alert and blood cultures, time between alert and serum lactate, inpatient mortality, rate of transfer to intensive care unit.
Results:
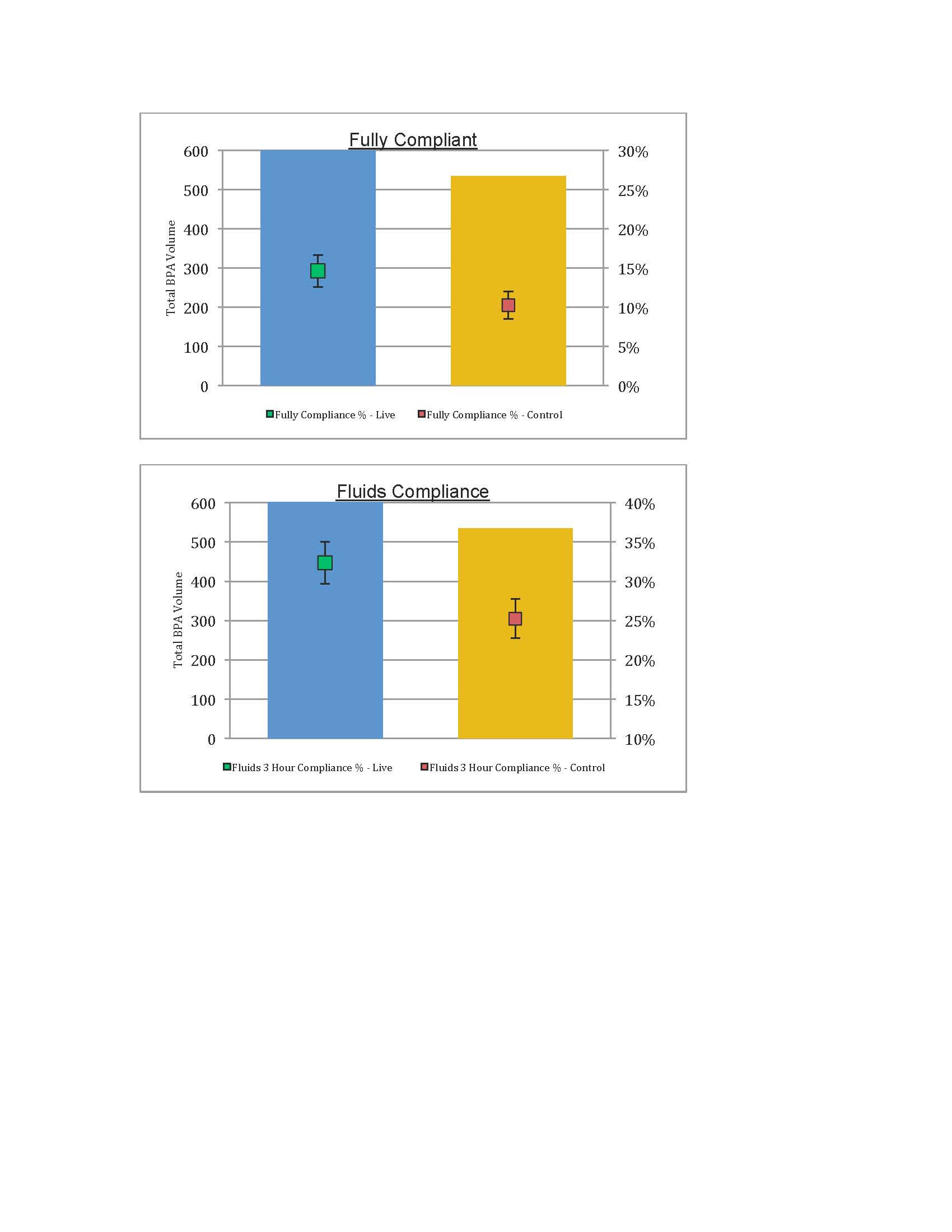
Patients in the intervention group (N=634) were more likely to receive the complete 3 hour sepsis bundle compared to the usual care group (N=535): 14.7% (95% CI: 12.7-16.7%) vs. 10.3% (95% CI: 8.6-12%, p=0.02). Other differences between intervention and usual care included intravenous fluids given within 3 hours was 32.3% (95% CI: 29.6-35%) vs. 25.2% (95% 22.7-27,7%, p=0.008), serum lactate within 3 hours was 82.2% (95% CI: 80-84.4%) vs. 78.5% (95% CI: 76.1-80.9%, p=0.11), blood-cultures done within 3 hours if not done in the past 24 hours was 71.1% (95% CI: 68.5-73.7%) vs. 69.9% (95% CI: 67.3-72.5%, p=0.65), antibiotics given within 3 hours 50.6% (95% CI: 47.1-53.5%) vs. 52% (95% CI: 49.1-54.9%, p=0.20), inpatient mortality 6.9% (95% CI: 5.4-8.4%) vs. 8.2% (95% CI: 6.6-9.8%, p=0.41), and transfer to ICU 7.1% (95% CI: 5.6-8.6%) vs. 5.2% (95% CI: 3.9-6.5%, p=0.19).
Conclusions:
An EHR-based severe sepsis alert resulted in a modest but significant improvement in several sepsis treatment performance measures. This type of alert is increasingly feasible given the widespread adoption of EHRs, though details in downstream clinical workflow are likely critical to impact clinical outcomes. Future alerts could likely be predictive rather than identify a clinical condition that has already occurred, though clinical workflow will remain critical to improve care.