Background: Introduction : A Medical Orders for Scope of Treatment (MOST) form, adopted by the state of Texas in 2014, is similar to Physician Orders for Life Sustaining Treatment (POLST/MOLST) form in other states. It translates patient preferences for CPR, critical care, assisted nutrition, and transfer between healthcare facilities into a physician order set. Previous research has shown that POLST forms are associated with goal concordant care at end of life. This form was integrated into the system-wide electronic health records of Baylor Scott and White Health System in 2015 and serves as an important tool for Advanced Care Planning. It is also used as a quality measure for physician compensation. Data from Texas since the statewide adoption of forms in 2014 is lacking.Objectives :1. Calculate rates of completion of MOST form at a Tertiary Academic Hospital and identify baseline predictors of completed form along with provider characteristics based on gender and specialty.2. Identify differences in directive of Attempt Resuscitation vs DNR based on patient race, location, and discussant of the form. 3. Explore contradictions between sections of the same form for resuscitation, degree of medical intervention, and assisted nutrition. The form was considered contradictory if choices within sections did not align to indicate fully conservative or aggressive care.
Methods: Single center observational retrospective study. Electronic medical records were queried for patients over 60 years old who were established patients at a tertiary academic hospital in Texas and had at least one inpatient admission at the same hospital in 2017. Patients with an external PCP were excluded. Follow up period was 1 year or until date of death.
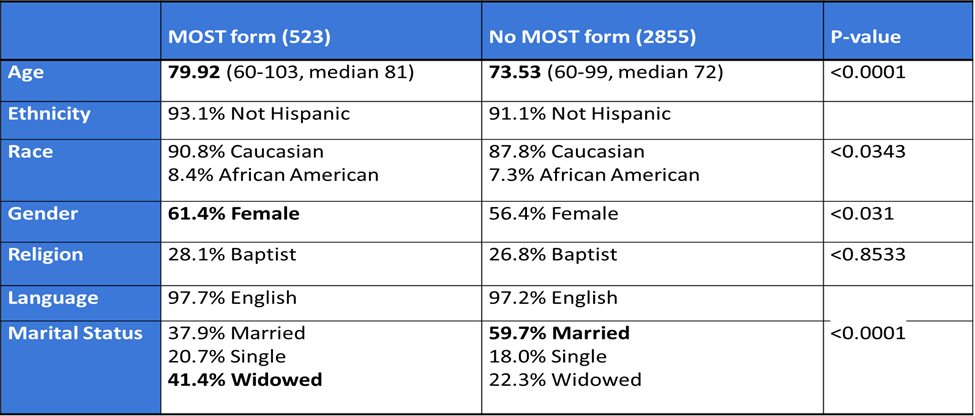
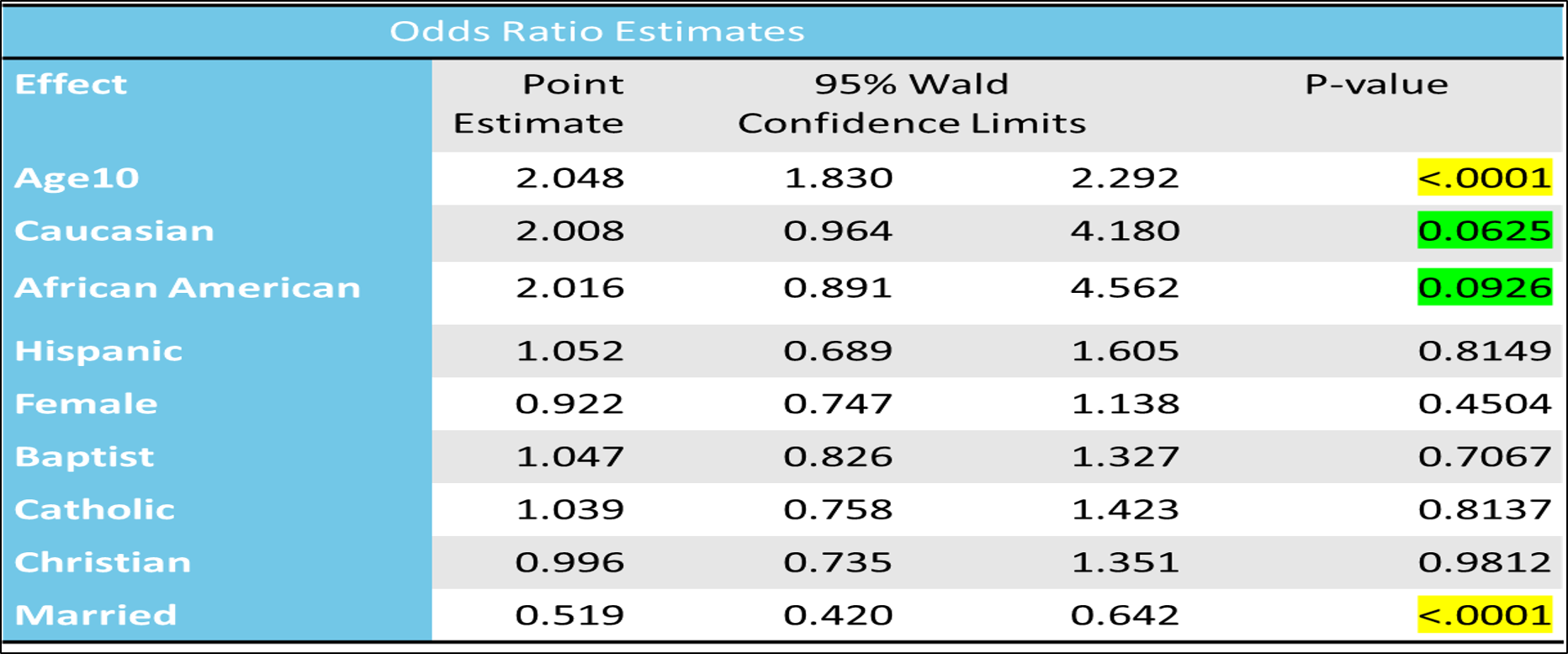
Results: Of 3377 patients, 523 (15.4%) had a MOST form completed. In the logistic regression analysis, age, marital status were predictors of MOST form completion with p values reaching statistical significance. 57.2% of patients with completed forms chose DNR. Difference in DNR vs Attempt resuscitation significant for: Race, location of completion, and discussant. Forms were completed by female provider 67.7% of the time, in the inpatient setting 52.6% of the time, and by a geriatric specialist 45.8% of the time. 155 (29.6%) of total forms were contradictory with greater number of contradictions when patients chose DNR (18.9%) vs Attempt resuscitation (10.7%).
Conclusions: Despite being recognized as a quality and pay for performance measure, rates of MOST form completion were low. The most common choice for resuscitation within completed forms was DNR. Disparities due to race exist. Approximately a third of the forms indicated contradictions in goals of care. Contradictions in forms highlight the gaps in communication around advanced directives and end of life care between patient and provider. This necessitates process measures to improve advance care planning, patient provider communication, and illness understanding in seriously ill patients.