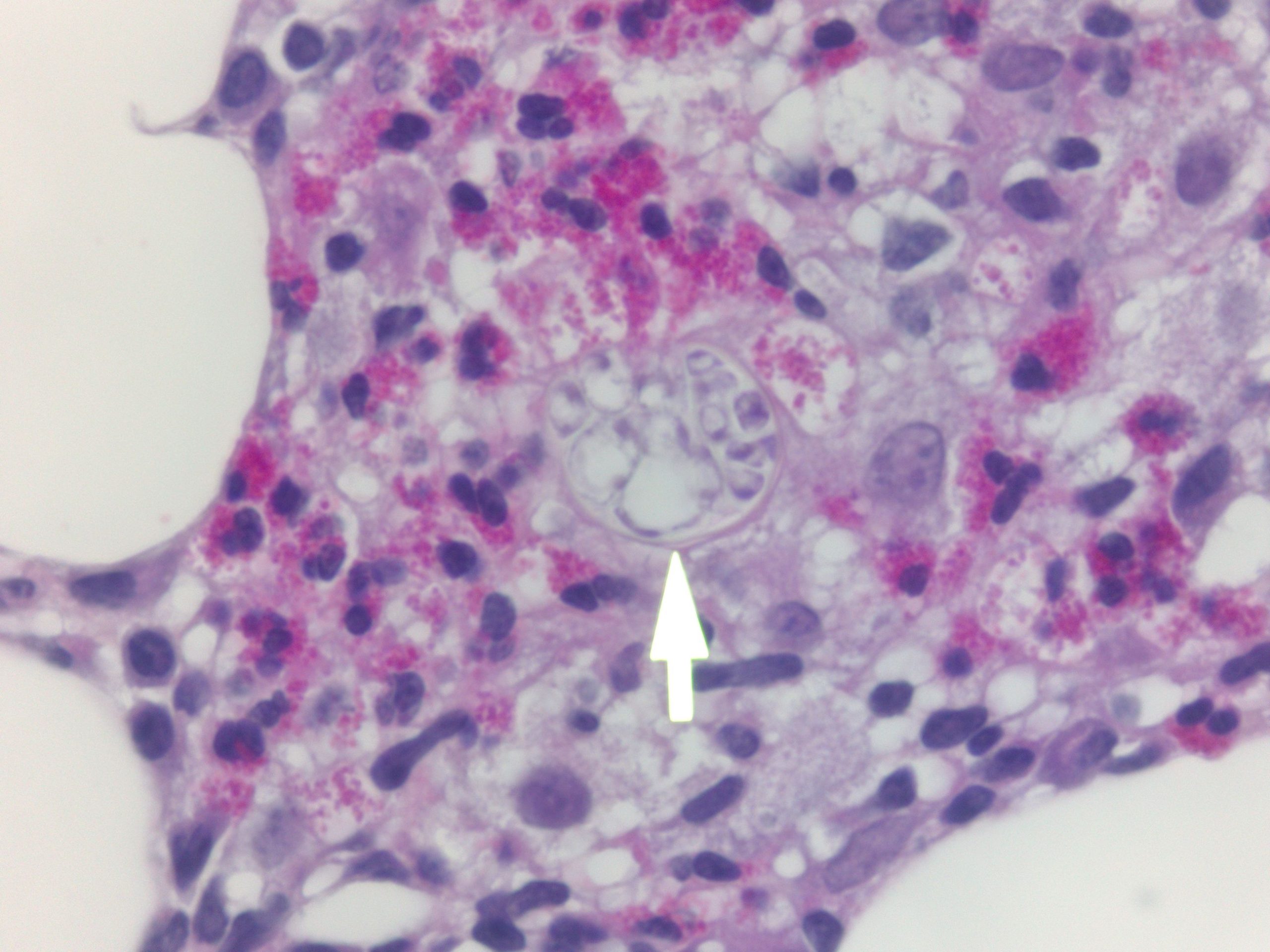
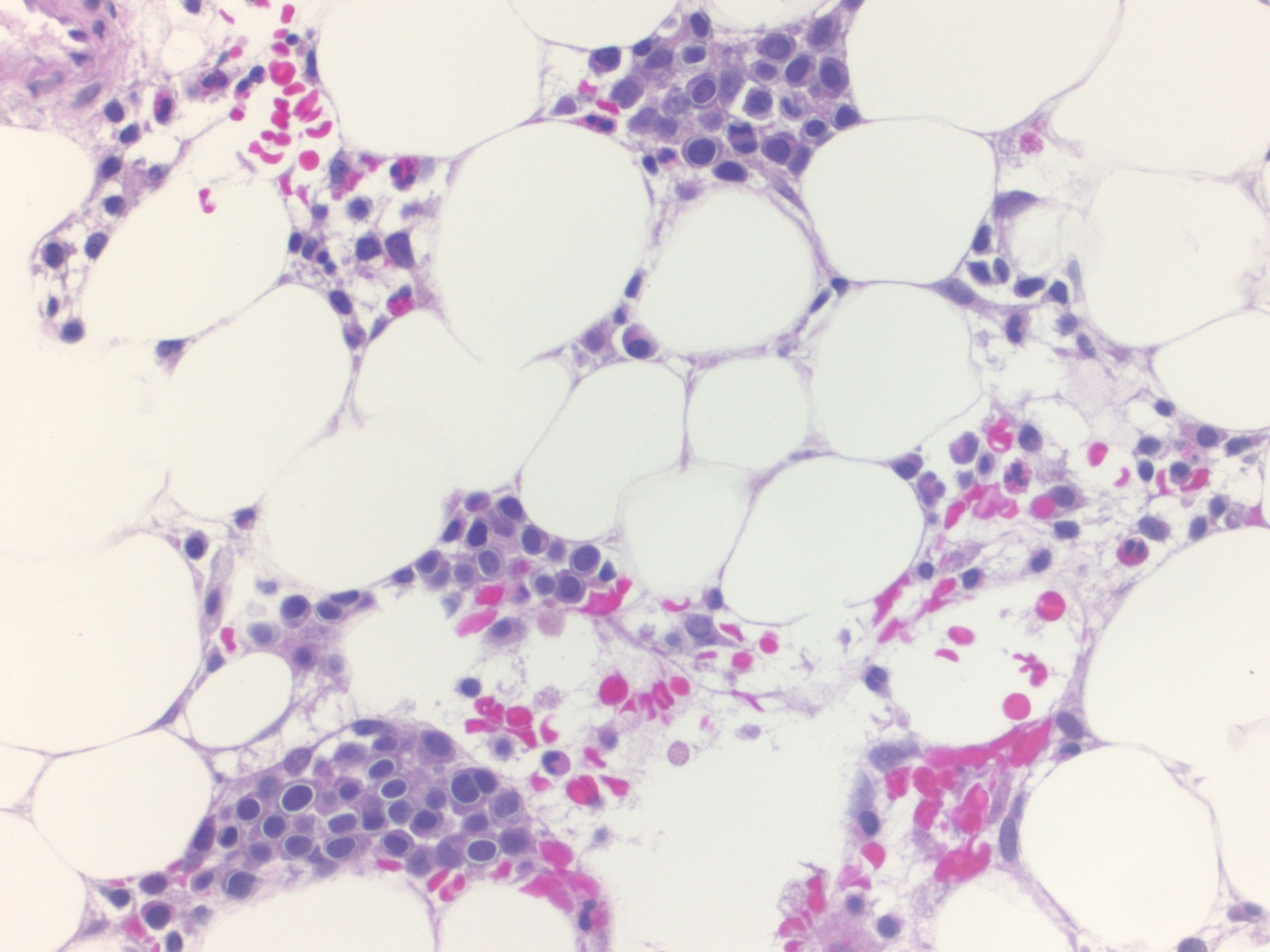
Case Presentation: Patient is a 60-year-old male with past medical history of Ledin’s factor V deficiency who presented to the ER with complaints of fever, chills, and weakness. His symptoms started with a headache, cyclical fevers, and violent rigors lasting several minutes. With the onset of rigors, patient progressed to develop ascending weakness. In the ER, the patient was febrile, tachycardic, and hypotensive. His initial physical exam showed that he was profoundly weak as his motor strength in the lower extremities was 3/5, and 4/5 in the upper extremities. Reflexes were absent in the lower extremities. Initial labs showed he had a very low white blood cell count of 1.5. Leucocytopenia was primarily neutropenic but absolute eosinophils were elevated at 14.1. His initial workup of HIV, COVID-19, and influenza were all negative. Patient was initially admitted to the ICU for pressor support but was able to be weaned. Neurological and other basic workup was negative but infectious disease started Diflucan after positive cocci titers. However, no clinical improvement was observed after several days. WBC count from admission had not improved, even worsening to the point of requiring neutropenic precautions. Hematology/Oncology was consulted and initiated a review of patient’s history. In the records review, it was found he had pancytopenia for four years. Bone marrow biopsy was ordered for in-hospital evaluation and after several days, came back positive for hairy cell leukemia with cocci spherules seen in the bone marrow. After diagnosis, the patient was transferred for inpatient chemotherapy.
Discussion: This case is complicated by the dual disease process of hairy cell leukemia and disseminated coccidioidomycosis. Prior to the hospitalization events, the patient had been asymptomatic and his abnormal neutrophil count had been his only lab value that showed any indication of the underlying malignancy. It is only when he developed an infection secondary to the cancer, that his disease could be discovered.Neutrophils have a well-understood role in immunity against coccidioidomycosis. As phagocytic cells, they act on the arthroconidia of cocci as well as immature spherules, able to kill the fungal particles. They are also the most numerous innate immune cells and often first responders to infection. One of the primary features of hairy cell leukemia is the depletion of bone marrow proliferated cells, which caused this patient’s neutropenia. This depletion likely went on for several years, depleting the patient critically and leading to infection. Not only did the hairy cell leukemia likely contribute to the coccidiosis dissemination, but due to the infectious process, his leukemia was masked. The patient’s symptoms were not suspicious of a neoplastic cause- his cough, diarrhea, fevers, and myalgia all indicating a more infectious etiology. However, once he was diagnosed with coccidioidomycosis and treated but continued to decline, clinical suspicions prompted a further workup.
Conclusions: This case demonstrates the importance of a broad differential in a non-specific presentation. The patient’s symptoms presented as an infectious or neuropathic etiology and the initial workup reflected these assumptions. However, as patient continued to decline, the workup had to adapt and change to determine the true cause of his symptoms. Although the diagnosis of coccidioidomycosis was correct, the clinical picture remained unclear until hematology/oncology pursued a widened differential.