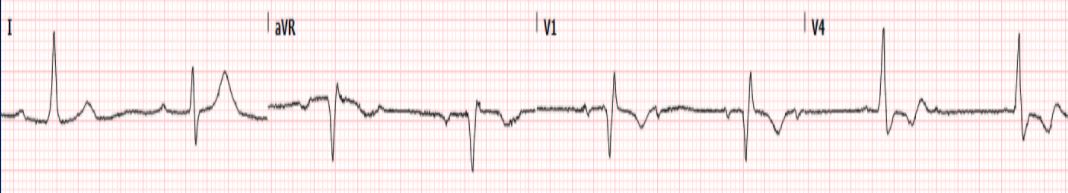
Case Presentation: A 37-year-old male with anxiety presented to the ED in Maine after a week of warmth and irritability, followed by sudden onset nausea and vomiting, epigastric and chest pain with left shoulder radiation, and palpitations. He denied COVID exposures, loss of taste or smell, shortness of breath, dysphagia, changes in weight, or skin rashes. He had no known tick exposures but did work outdoors. Physical exam was unrevealing except for heart rate from 30-120bpm. Telemetry showed variable AV blocks including 1st, 2nd (type I) and 3rd degree (see image). CTA chest and CT abdomen/pelvis demonstrated no acute findings. Patient underwent a negative echocardiogram. After non-diagnostic stress test, cardiac catheterization showed patent coronary arteries. Lab evaluation included; WBC 11k/mm3, Hgb 11g/dL, ALT 120U/L, AST 72U/L, Alkaline phosphatase 333U/L, Troponin 0.01ng/mL (x2), COVID-19 negative. TSH was suppressed at 0.02mIU/L, free T3 elevated to 14pg/mL and free T4 elevated at 4.6ng/dL, anti-TPO Abs were negative. Ultrasound showed no masses within the thyroid. Patient was initiated on methimazole, while beta blocker was held due to intermittent bradycardia. Of note, initial Lyme PCR was negative, though Lyme IgM was later positive. The patient was treated for concurrent diagnoses of Lyme carditis and hyperthyroidism. He received IV ceftriaxone until AV nodal blocks resolved, and was then transitioned to PO doxycycline for a total 21 days which was curative. With improved heart rate he was started on propranolol along with methimazole and endocrinology follow-up was arranged.
Discussion: Workup of this patient with variable dysrhythmias resulted in multiple diagnoses including Lyme carditis and hyperthyroidism. Lyme carditis may result in conduction abnormalities including fascicular blocks, QT prolongation or AV blocks which can progress from 1st through 3rd degree over 2 weeks time. Direct cardiac invasion by spirochetes leads to inflammation and scarring which disrupts conductivity. Lyme disease is a tick-borne zoonotic disorder endemic to New England, caused by the spirochete Borrelia burgdorferi. Only 30% of patients can recall tick exposure. Lyme may present with fevers, headache, target rash, body aches, facial paralysis, meningitis, or carditis. Lyme PCR negative status may give false reassurance; however, this can be extremely transient. Western blot with a positive IgM, +/- IgG, is most consistent with Lyme carditis. The tachycardia experienced by this patient is uncommon with Lyme carditis and was attributed to concurrent hyperthyroidism. It should be noted that amino acid sequence homology between thyroid autoantigens and Borrelia proteins has been reported and may be capable of triggering autoimmune thyroid disease in persons with certain HLA-DR alleles. Borrelia itself has also been shown to have affinity for the TSH receptor which could, in theory, lead to T4 release and TSH suppression without thyroiditis or subsequent hypothyroidism.
Conclusions: Varying degrees of AV heart block with tachy-brady arrhythmia were seen in this case, leading to concurrent diagnoses of Lyme carditis and hyperthyroidism. Lyme carditis should be considered in patients in endemic areas without other likely etiologies of heart block. While seemingly unconnected, we postulate that a unifying diagnosis may be supported by Borrelia activation of the thyroid gland.