Background: Written discharge instructions frequently lack guidance on how patients should address problems and questions that arise at home, and this represents an opportunity to enhance discharge safety and prevent readmissions. This study aimed to increase the number of discharge instructions that included anticipatory guidance and self-management among patients discharged from internal medicine teaching services at an academic medical center.
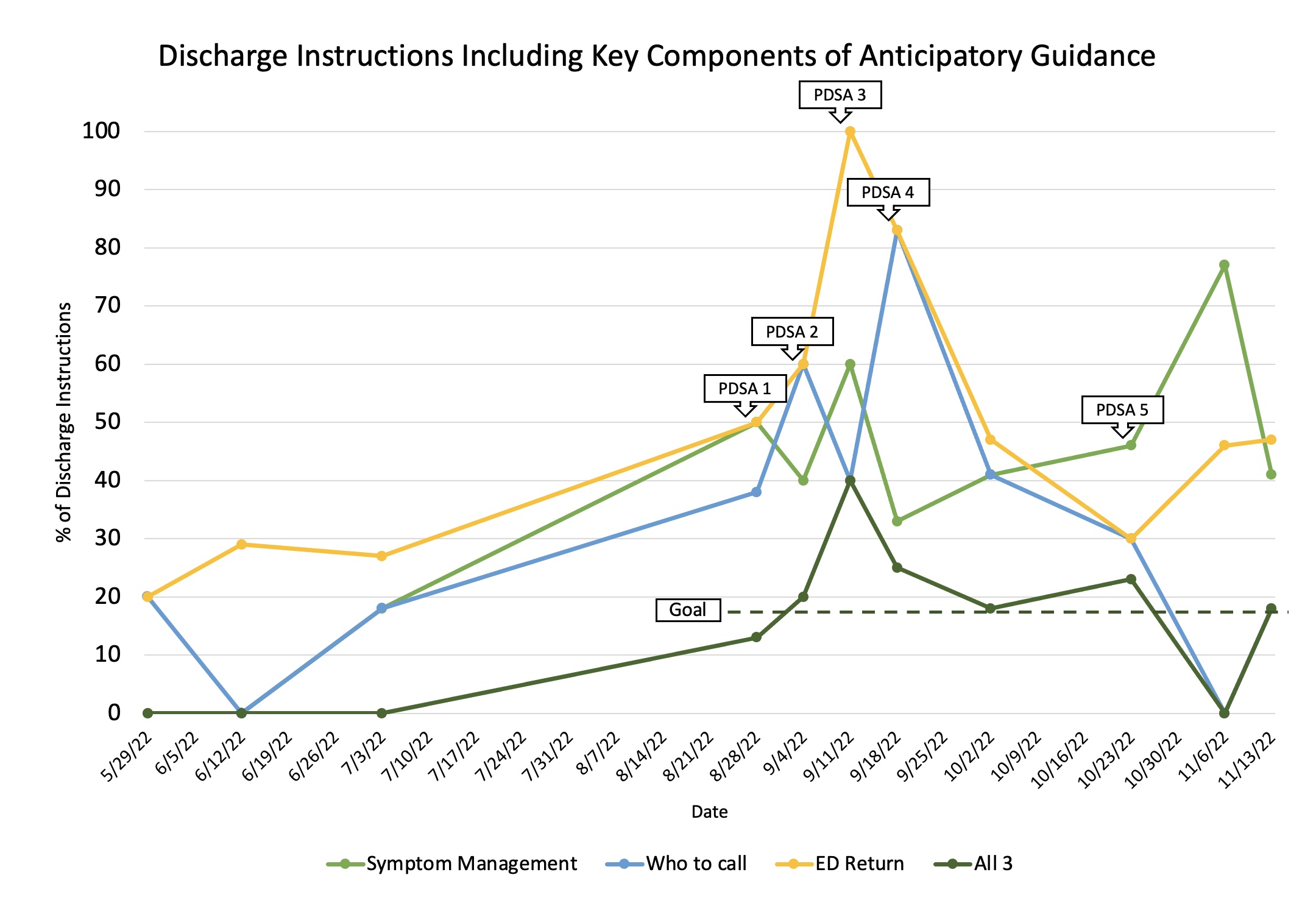
Methods: Baseline data was collected through manual chart review of a sample of medical patients discharged to home starting in May of 2022. Discharge instructions were evaluated for 3 primary components: how to manage symptoms at home, who to call with questions, and when to return to the emergency department. A new discharge instruction SmartPhrase (SP) was created and made available to residents which has prompts for the inclusion of the 3 components outlined above. Five iterations of this SP were completed through PDSA cycling based on data analysis and resident feedback, which was obtained via survey.
Results: Discharge instructions with all 3 aspects of anticipatory guidance increased from 0% in the pre-intervention period (n=23) to 18% in the post-intervention period (n=90). The specific components of anticipatory guidance each increased: symptom management instructions from 9% to 48%, information on who to call from 13% to 36%, and emergency room return precautions from 26% to 53%. The SP was utilized for 31% of patients in the post-intervention period. Only 6% of patients received the 3 aspects of anticipatory guidance when their instructions were created from a standard template, as opposed to 43% of patients whose instructions were created with the SP. Of residents who used the SP, 81% thought it added value to their instructions and 44% agreed it added new information which they otherwise would not have included.
Conclusions: Anticipatory guidance and patient self-management are vital components to incorporate into discharge instructions for home-going patients. We focused on 3 primary components that were rarely incorporated into discharge instructions prior to our intervention, and were never all 3 incorporated. Through the development of our novel SP, which has prompts for each element, we significantly increased inclusion of these important concepts, both individually and collectively for all 3. Despite residents reporting added value from using the SP, it was utilized in less than half of discharges in the post-intervention period. Future efforts will focus on standard integration of the SP into clinical workflows to further increase utilization rates.