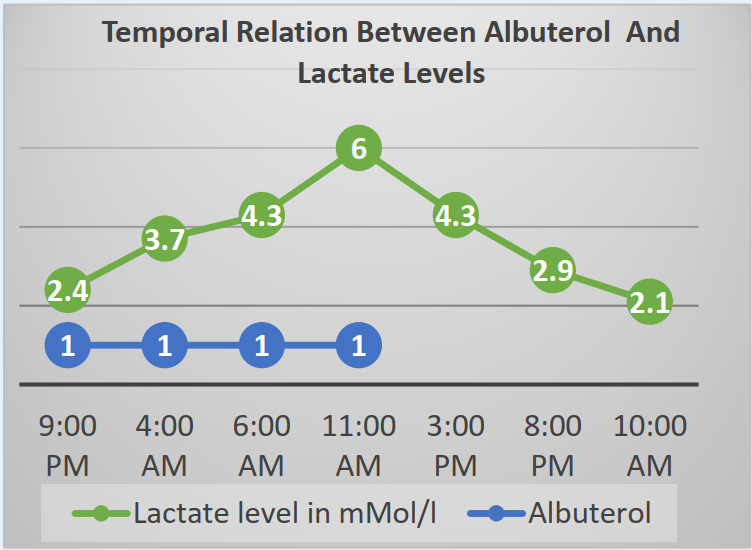
Case Presentation: Type A Lactic acidosis is commonly caused by decreased oxygen delivery and poor peripheral perfusion. Type B lactic acidosis ensues in absence of hypoxia or tissue hypoperfusion, mostly occurring in alcoholism, mitochondrial dysfunction, medications like metformin. We present an unusual case of Type B lactic acidosis induced by nebulized albuterol in the treatment of a COPD exacerbation. A 65-year-old woman with GOLD stage II COPD and a 60 pack-year smoking history presented with shortness of breath associated with increased cough and sputum production. Upon presentation, she was hypertensive (BP 170/84), tachycardic (HR 114), afebrile (temp 99.4 F), and with a peripheral oxygen saturation of 92 % on room air. A diagnosis of acute COPD exacerbation was made based on bilaterally decreased air entry with expiratory wheeze on chest auscultation, increased dyspnea, and cough with sputum production. Her initial blood work was unremarkable except for elevated lactate at 2.4 mMol/l (upper limit of normal 2.2 mMol/l). She received 2 doses of nebulized 3 mg – 0.5 mg albuterol- ipratropium over 1 hour, resulting in symptomatic improvement. She also received azithromycin and prednisolone. Her lactate continued to trend up and peaked at 6.0 mMol/L. The most common causes of lactic acidosis were ruled out. She did not have evidence of sepsis considering lack of hypotension, hypoxia, fever, leukocytosis, or identified source of infection. There were no signs of end-organ hypoperfusion supported by normal liver and kidney functions and warm peripheries. She denied abdominal pain or melena concerning for bowel ischemia, and the physical exam did not reveal any areas of gangrene. She was not prescribed metformin. Initially, lactate elevation was attributed to respiratory muscle fatigue but subsequently worsening lactate levels despite improving respiratory status pointed towards albuterol as a potential culprit. Discontinuation of albuterol resulted in the normalization of lactate levels. Upon discharge, she was instructed to use an albuterol rescue inhaler solely as needed.
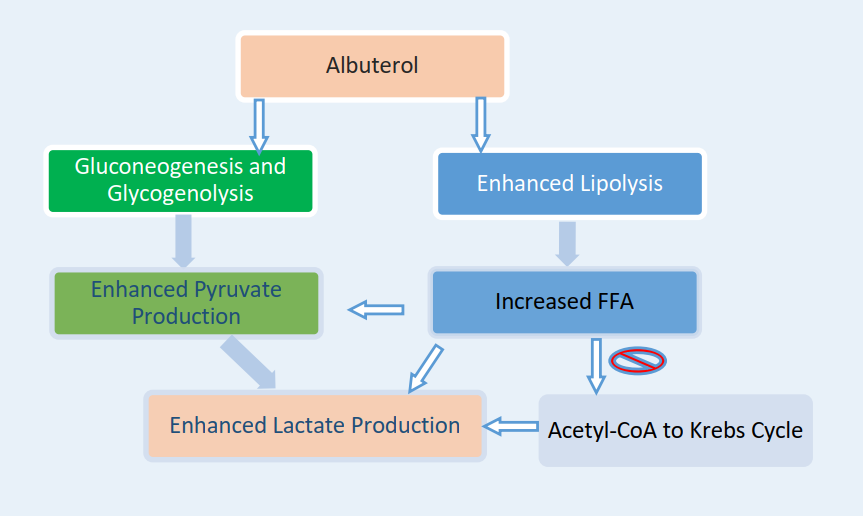
Discussion: Albuterol induced lactic acidosis has been identified as a potential complication of COPD exacerbation treatment resulting in type B lactic acidosis with a normal anion gap. One proposed mechanism for albuterol-induced lactic acidosis is overwhelmed oxidative metabolism through an increase in glycolysis and glycogenolysis. Another is via enhanced lipolysis, production of free fatty acids and acetyl-CoA, shifting pyruvate from the citric-acidy cycle, and leading to increased lactate production. Beta-adrenergic mediated inhibition of pyruvate dehydrogenase further impedes the conversion of pyruvate to acetyl CoA. Glucocorticoids, typically used in the treatment of COPD exacerbation, increase the sensitivity of Beta-adrenergic receptors, worsening lactic acidosis.
Conclusions: In our case, we highlight the importance of recognizing albuterol as a potential culprit behind the paradoxical worsening of lactic acidosis when using albuterol based breathing treatments for COPD exacerbation.