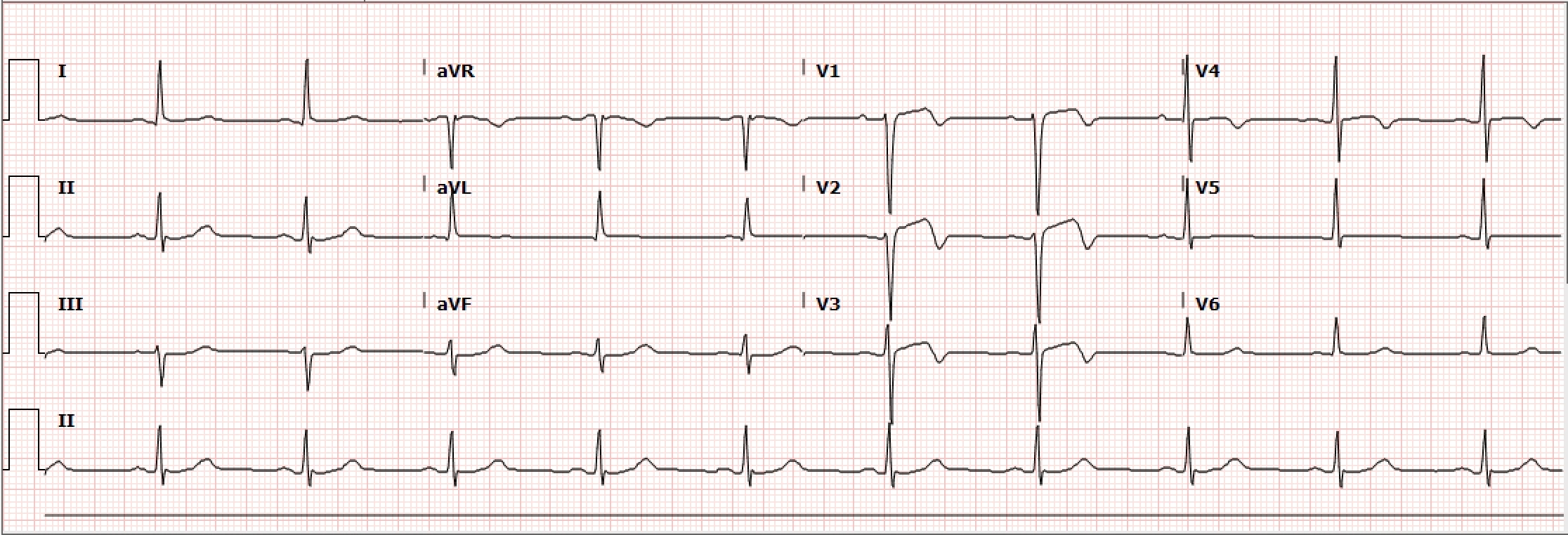
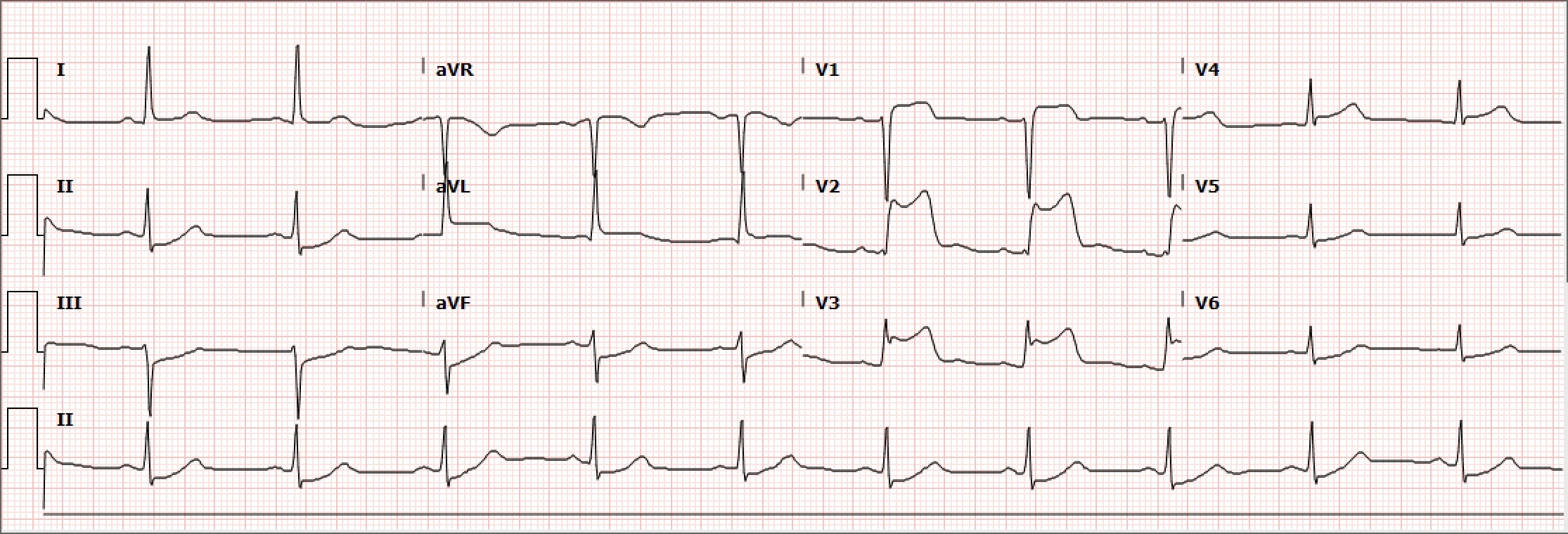
Case Presentation: A 52-year-old male with type-2 diabetes mellitus, hypertension, and tobacco use presented to the emergency department due to chest pain radiating to the left shoulder that began 24-hours prior. Upon arrival, he was afebrile, heart rate was 71 bpm, blood pressure was elevated to 193/117 mm Hg and had a normal oxygen saturation on room air. On initial exam, he was ill-appearing and diaphoretic. Electrocardiogram (ECG) was obtained demonstrating repolarization abnormalities in leads V1-V3. Sublingual nitroglycerin and aspirin 162mg were given, and continuous IV nitroglycerin was started. Chest X-ray was unremarkable. Initial Troponin-T was 0.05 ng/mL. Second and third serial ECGs were unchanged, however, 3 hours after arrival, the chest pain worsened and repeat ECG demonstrated 1mm ST segment elevation and biphasic T-waves in V1-V3, T wave inversion in V4, and T-wave flattening in V5 and V6 concerning for Wellens’ Syndrome. Heparin drip was initiated and the patient was admitted to the Coronary Care Unit for management of non-ST-segment elevation myocardial infarction (NSTEMI). On arrival, the patient again complained of intense left-sided chest pain and was diaphoretic. ECG was obtained and demonstrated ST-segment elevation in V1-V3 and reciprocal ST-segment depression in leads II, III, and aVF, confirming diagnosis of STEMI. The patient was taken urgently for percutaneous coronary intervention (PCI) where he was found to have total occlusion of the proximal Left Anterior Descending (LAD) artery. A 3.5mm x 28mm drug-eluting stent was successfully placed without residual stenosis. ST-segment elevation resolved following PCI, and the patient was started on dual anti-platelet therapy, atorvastatin, and metoprolol. He was seen 1 month later and was doing well at that time.
Discussion: Wellens’ sign was first reported in the literature in 1982 by de Zwaan and Wellens. They observed a pattern of ST-T segment changes among patients hospitalized for unstable angina that were suggestive of critical LAD stenosis.[1] Criteria for Wellens’ sign include the following: (1) Either biphasic T-waves in V2 and V3 (Type A) or deep and symmetrical T-wave inversions in V2 and V3 (Type B); (2) ECG without Q-waves and no significant ST-segment elevation, and with normal precordial R-wave progression; (3) History of anginal chest pain; and (4) Normal or minimally elevated cardiac enzyme levels.[2] When these criteria are met, the positive predictive value of Wellens’ sign is approximately 86%. It is important to note that these criteria may be present during pain free intervals.[3] Wellens’ syndrome results from temporary obstruction of the LAD, usually due to atherosclerotic plaque rupture, subsequently followed by clot lysis or disruption of the occlusion before infarction occurs. Thus, although Wellens’ syndrome represents a pre-infarction state, there is high risk for progression to extensive myocardial infarction (MI) of the anterior wall and possibly death. Treatment of patients with this syndrome includes aspirin, nitroglycerin for pain, and beta-blockers if appropriate, as well as hospitalization due to the acuity and potential for evolution. The key issue is understanding that patients with Wellens’ syndrome should undergo coronary angiography and that stress testing is contraindicated, as it may provoke MI.[4]
Conclusions: Recognizing the ECG findings of Wellens’ syndrome is essential to proper management and emergent intervention to avoid anterior wall MI.