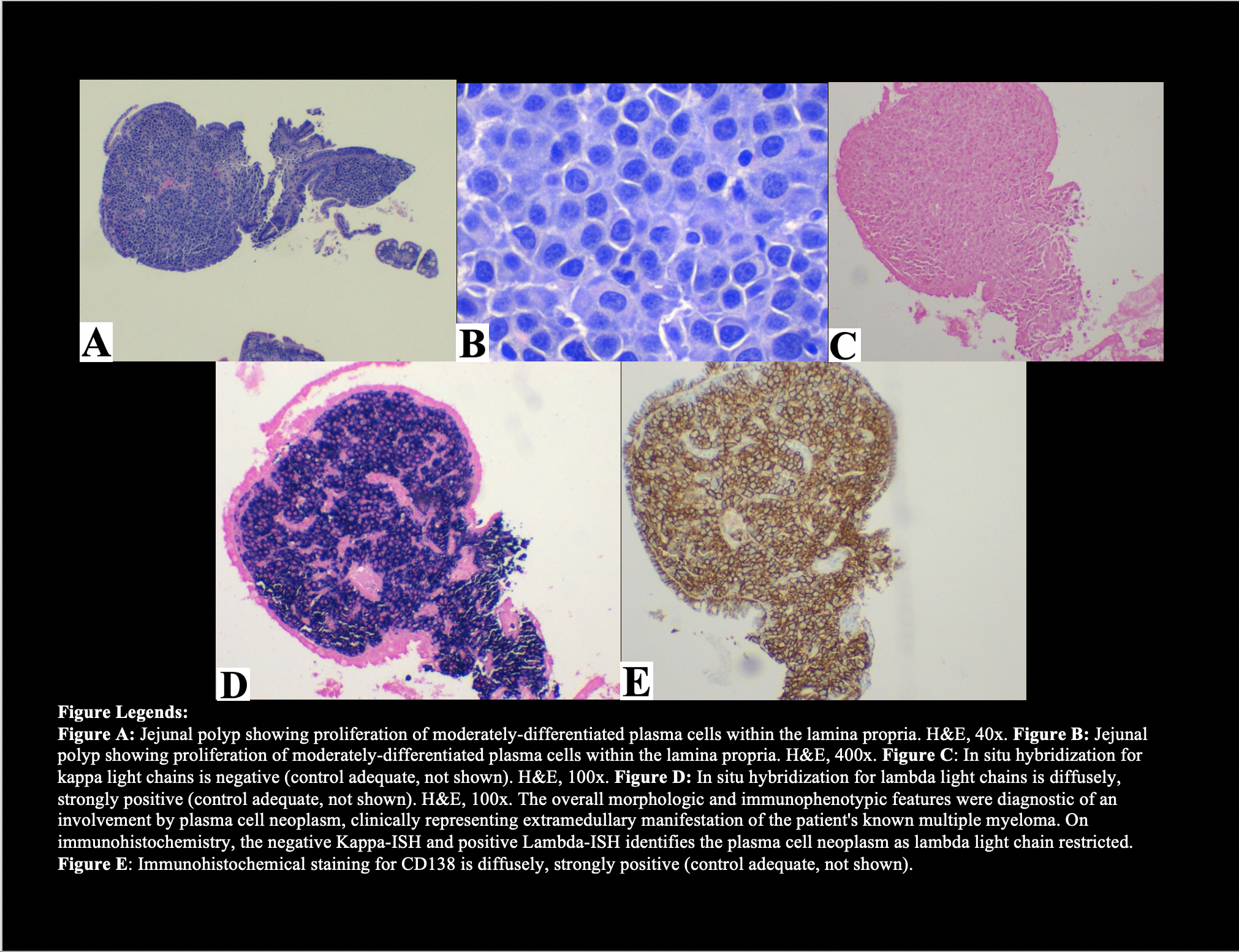
Case Presentation: A 49-year-old male presented with shortness of breath, fatigue and four weeks of dark stools. He had previously been diagnosed with IgG lambda multiple myeloma (MM) with renal insufficiency and hypertension. He had MM disease progression despite completing chemotherapy and had declined further treatment. Physical exam revealed an ill-appearing, pale mane with a subcutaneous, nontender right upper quadrant abdominal mass upon palpation. Rectal exam revealed melena. He was found to be severely anemic with a hemoglobin of 4.0 g/dL requiring blood transfusions.. Esophagogastroduodenoscopy (EGD) and colonoscopy did not reveal a source of bleeding. Video capsule endoscopy showed multiple small bowel polyps of variable sizes mainly in the duodenum and jejunum with some appearing ulcerated with active bleeding in the proximal to mid-jejunum. Anterograde single balloon enteroscopy revealed no active bleeding and multiple polyps. Fine needle percutaneous aspiration biopsy of the subcutaneous abdominal mass confirmed plasma cell neoplasm (see Figure). The patient’s bleeding spontaneously resolved, and initiation of MM therapy was recommended.
Discussion: Extramedullary plasmacytomas (EMP) constitute less than 5% of all plasma cell neoplasms(1) and can be classified as primary or secondary. GI involvement most frequently includes sites such as the stomach, liver and colon(2,3). A large retrospective study showed that gastrointestinal plasmacytoma accounts for only 0.9% of cases in the course of multiple myeloma(4). Mechanisms of extramedullary spread in MM likely involve direct extension from skeletal tumors or hematogenous spread(5,6). Abdominal pain is the most common manifestation. Other nonspecific symptoms include those related to intestinal obstruction and GI bleeding(2). In the setting of new GI symptoms, evaluation for EMP should be considered especially in patients with known history of multiple myeloma. Work up includes laboratory studies with peripheral blood cell count, hepatic and renal function tests. Due to blood loss from vascular or ulcerated bleeding lesions, an iron deficiency anemia may be expected. Imaging such as CT or PET scan can elucidate size and location of the EMP(6). EGD can show EMP in stomach or duodenum and allows for performance of biopsies. Differential diagnosis includes adenocarcinoma, lymphoma, amyloidosis and metastatic neoplasms(7). Histopathological, immunohistochemical or immunophenotypic analysis confirms the diagnosis(5). Once diagnosis is achieved, the goal is to determine if the lesion is primary or secondary EMP. Primary EMP of the small intestine has a more benign clinical course, while secondary EMP reveals progressive systemic involvement of multiple myeloma(2). Management may include surgery, radiotherapy and/or chemotherapy. Secondary EMP due to multiple myeloma is usually seen in a later stage and confers a poor prognosis(4,8,9).
Conclusions: Clinical suspicion for extramedullary plasmacytomas is infrequent due to the nonspecific manifestations and rarity of cases. However, the above case demonstrates the need for evaluation in patients with MM who present with GI bleeding. Diagnosis is established following biopsies and histopathological confirmation. Secondary EMP in the setting of MM indicates a poor prognosis. Consequently, clinical awareness of extramedullary involvement of MM is strongly encouraged, as early detection will impact medical therapy.