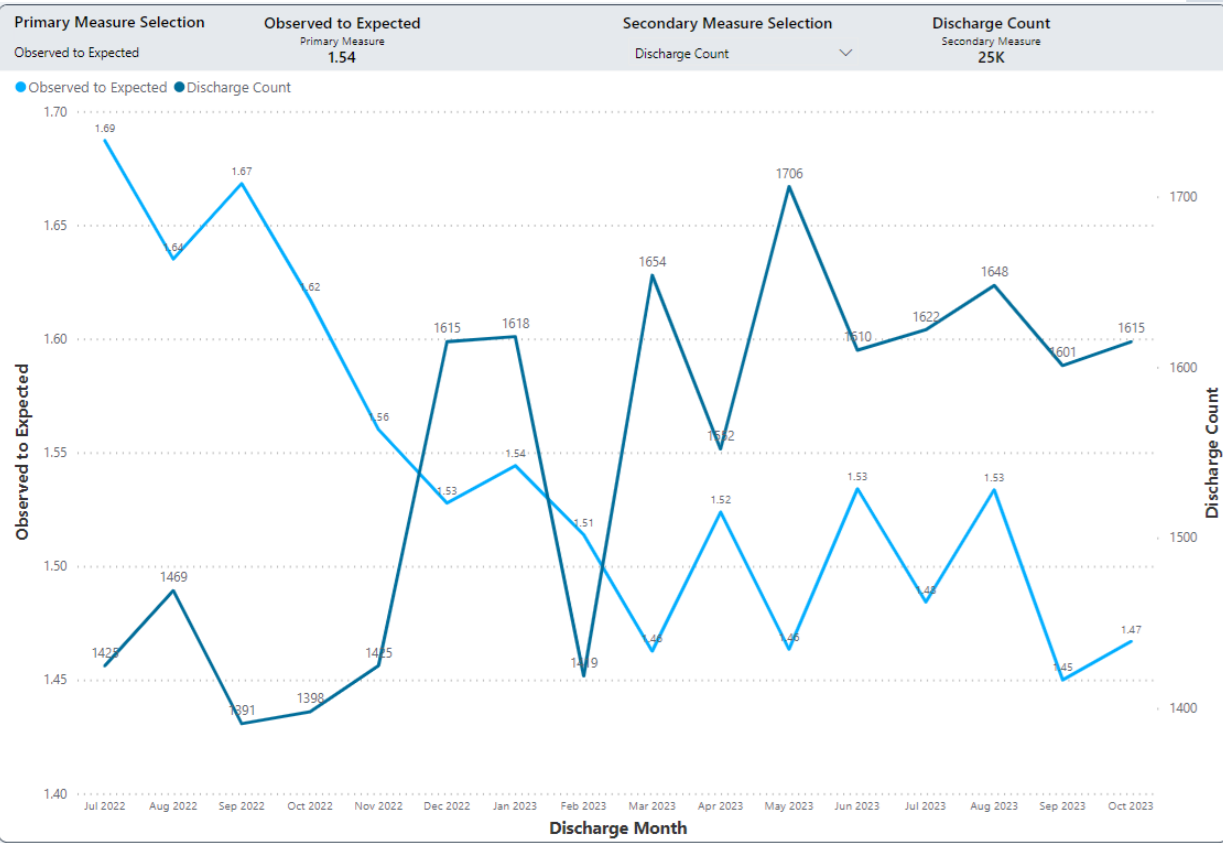
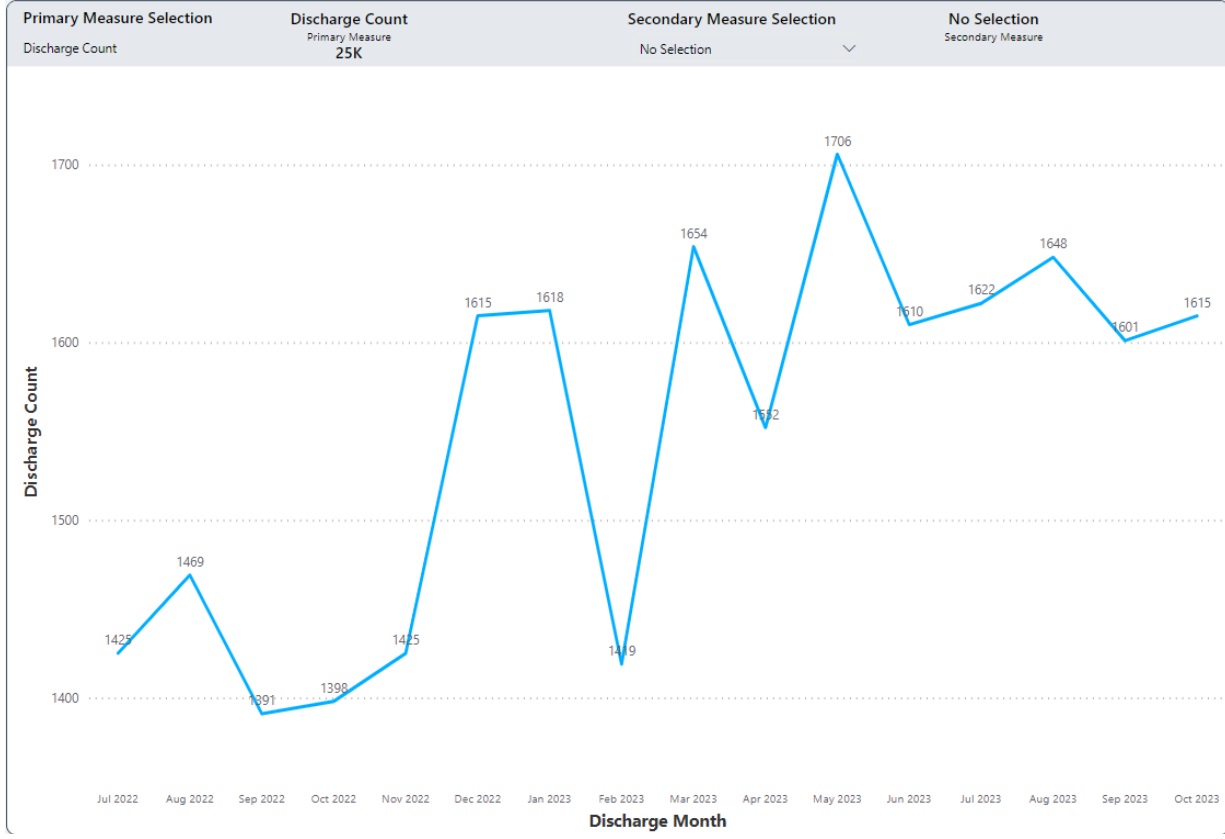
Background: The leadership of our academic hospital medicine group designed a geographic rounding intervention with the goal of improving patient-nursing communication, decreasing hurdles in discharging patients and eventually leading to reducing patient length of stay and increasing discharge rate. Our quantitative analysis compared the pre-intervention and post-intervention time periods with regard to observed to expected discharge O/E ratio.
Methods: The goal of assigning hospitalists to a specific nursing unit (geographic assignment) was to ensure that more than 80% of their assigned patients were located at their assigned unit. We established meetings for multidisciplinary teams twice daily. We have been analyzing the effects of the interventions mentioned above on various outcomes in two hospitals in Oklahoma City. The discharge process was monitored on a monthly basis. We evaluated the observed discharge date against the anticipated Geometric Mean Length of Stay (GMLOS).
Results: We observed the trend of significant decline in length of hospital stay and drop in Observed to expect the discharge O/E ratio. It was found that these interventions had a positive effect on converting observation status admissions to inpatient status.
Conclusions: Geographic rounding and multidisciplinary meetings have the potential to increase communication between physicians and nurses, shorten inpatient stays, and expedite discharges.