Background: The emergence of hospitalists over the last 25 years as leaders in quality, safety, and value-based care has resulted in improvements in hospital throughput and reduction of in-hospital complications (1). The keys to success are standardizing clinical pathways and interdisciplinary collaboration. At Tampa General Hospital (TGH), our hospitalist team observed significant variability in the care of post-operative cardiothoracic (CT) surgery patients and increased length of stay (LOS). From 12/2021 to 11/2022 the average surgical LOS for postoperative patients was 10.8 days (Society of Thoracic Surgery data) and total LOS index (Vizient) was 1.19, well above the 20th percentile. For 2022, TGH also had 722 excess days for this patient population. On transfer of patients from the CT intensive care unit to the hospitalist floor, we identified a lack of standardized handoff as a major barrier to efficiency. In conjunction with CT surgery and critical care leadership, we developed a hospitalist co-management service (HCS) and a standardized care pathway with an aim to reduce surgical LOS by one day and LOS index by 0.3 days.
Methods: We developed a service agreement formalizing each provider’s responsibility throughout the care pathway. Our initial plan was to have hospital medicine consults placed 24-48 hours before a predicted transfer order rather than at time of transfer. This early relationship with the patient aimed to build trust and identify complex medical issues and discharge barriers earlier. After 90 days, we expanded the HCS to include all patients admitted to CT surgery, not just those admitted for elective CT surgery. We partnered with case management adding daily multidisciplinary rounds to our workflow, created a pharmacy pathway to improve faster therapeutic warfarin dosing, and built a hospitalist guide to CT surgery to update hospitalists’ knowledge on contemporary procedures, perioperative management, and surgical complications.
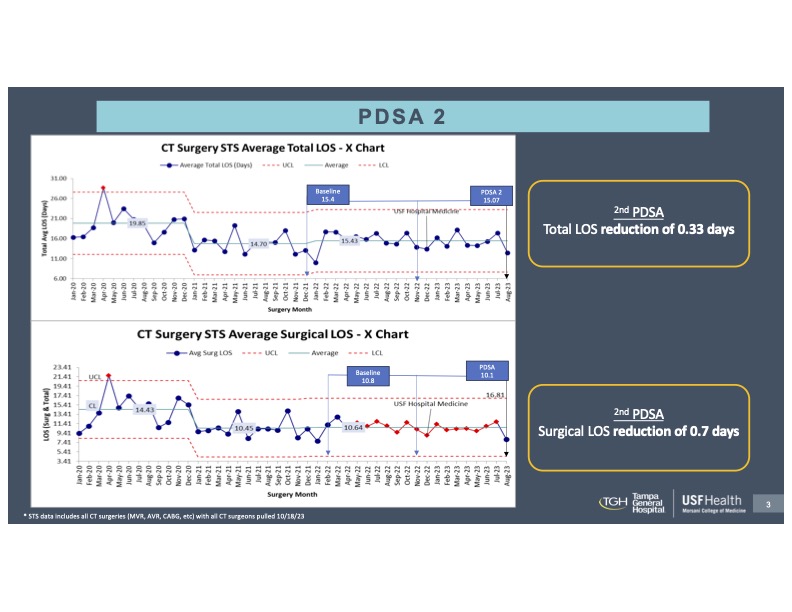
Results: In our first test of change in 90 days, we improved surgical LOS by 0.7 days (Figure 1). Our second PDSA confirmed a 0.33-day reduction in total length of stay and a 0.7-day reduction in surgical length of stay (Figure 2) with an average of 6.04 days saved a month after our first two PDSAs. Our outlier patient population staying longer than 14 days also decreased despite a higher case volume. Our HCAPS score, and balancing metrics were not significantly affected, nor was the Vizient LOS index (1.19 pre- and 1.18 post-intervention).
Conclusions: Although the literature is sparse, the co-management of complex surgical patients with hospitalists has previously been shown to improve efficiency and outcomes (2), specifically readmission rates, mortality, and length of stay (3). At our institution, the postoperative integration of the HCS helped to decrease LOS without affecting HCAPS scores and readmission rates. The earlier recognition of complex medical issues, barriers to discharge, and increased time to establish rapport are highlighting the need for hospitalist involvement in the postoperative period for CT surgery patients. Leveraging the partnership with surgeons, we are now developing clinical care pathways to standardize preop and postop workup and management, with a goal to reduce redundancy. With our continued work, we hope to contribute to existing evidence of the utility and value-add of HCSs, specifically in the CT surgery realm.