Background: In the South Bronx, 30% of the population lives with heart failure. CHF readmission andmortality rates surpass the national average in the Bronx. Our hospital serves anethnically diverse population, predominantly Hispanic and African American, many ofwho have a low socioeconomic status. Despite multiple interventions including educating patients about CHF Action Plan, ensuring all eligible patients are prescribed GDMT, referral for advanced cardiology care and post discharge care transitions, there was no discernible change in readmissions. Hence we aimed to evaluate patient related factors including social determinants of health (SDoH), Burden of Treatment (BoT) which provides a framework to illustrate and how interactions between patients, their healthcare systems, and their support networks can affect and exacerbate patients’ ability to manage chronic illness and quality of life among patients readmitted with CHF decompensation from April to May 2023.
Methods: All readmitted patients in the study period completed telephone survey questionnaires regarding SDoH, BoT using Patient Experience with Treatment and Self-management (PETS) measure which assesses the domains including ability to understand medical information, problem with managing medications including side effects, medical appointments, monitoring health, interpersonal challenges, medical and healthcare expenses, difficulty with healthcare services, role and social activity limitations and self-care causing physical and mental exhaustion and quality of Life using ED-5D.
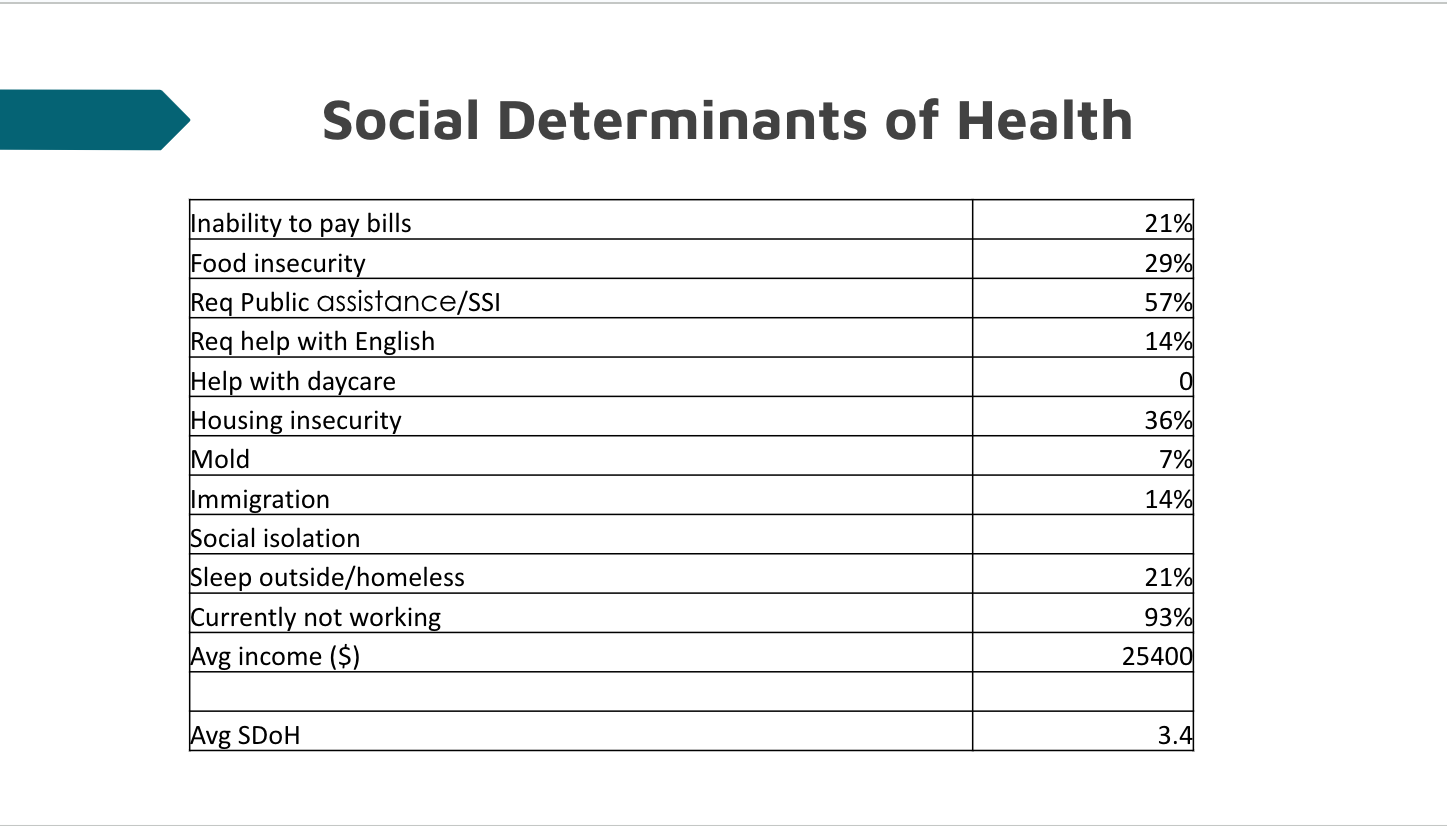
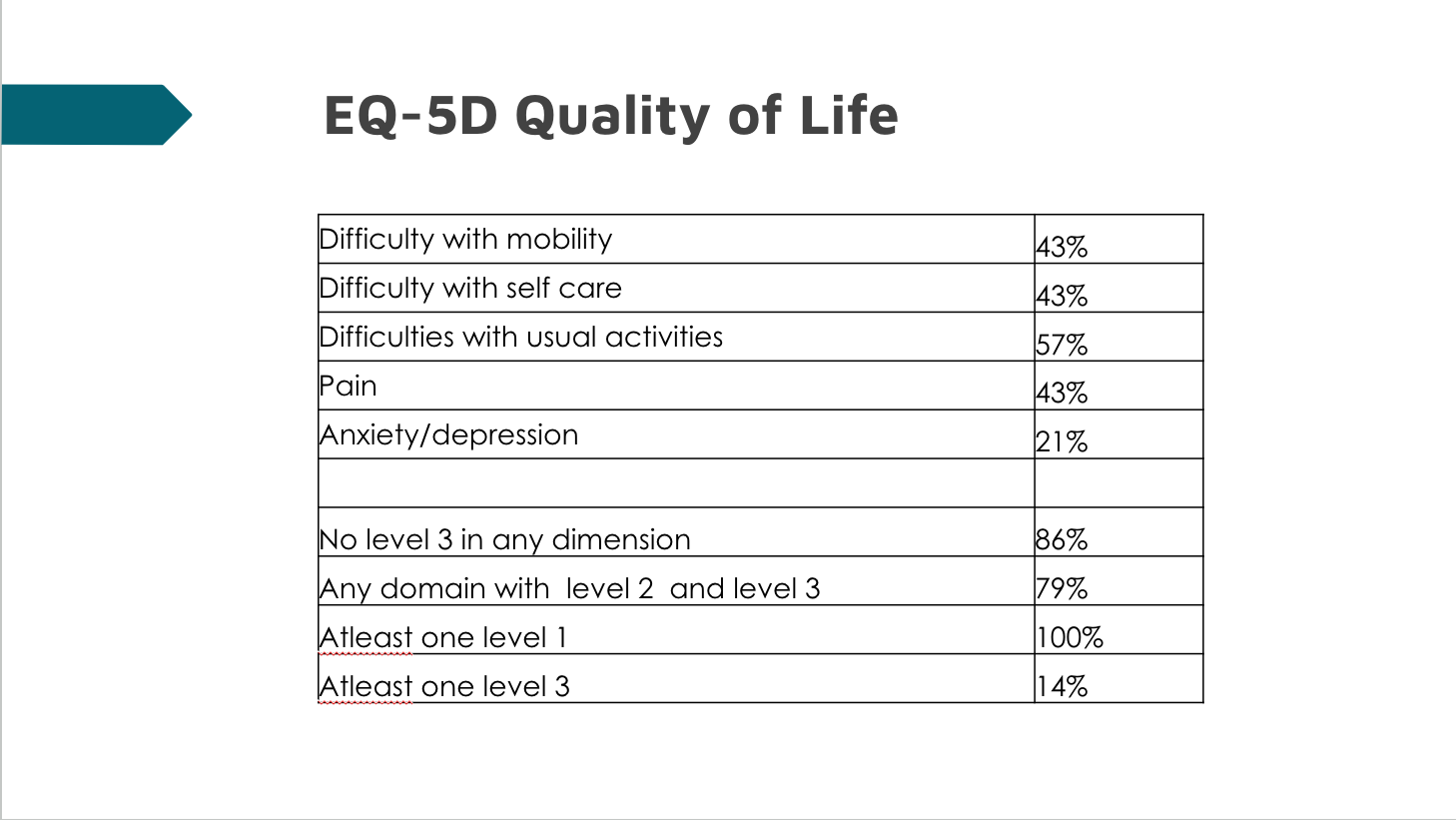
Results: Among the 25 participants, mean age was 66.7 years, 68% were male with 28% with high school/some college education, 55% preferred communication in Spanish and all of them had medical insurance. Most of them had HFrEF with a mean number of 4.88 comorbidities, 14% had underlying mental illness and 20% with substance use excluding alcohol and 20% with alcohol use disorder. Average SDOH burden per patient was 3.4, with 29% with food insecurity, 36% with housing insecurity, 21% homeless, 93% were currently not working, 21% had inability to pay bills and 57% were on public assistance. All patients have at least one domain involvement in QoL assessment with 79% having a level 2 or level 3 involvement suggesting moderate/severe disability and 21% had untreated anxiety and depression. BoT assessment showed 93% had physical and mental exhaustion secondary to selfcare, 86% had difficulty with health care services – including appointments, 86% had problems with medical and healthcare expenses and 86% had difficulty with learning medical information. 79% of patients perceived selfcare affected family roles and limited social activities. 64% were bothered by their medications. 43% had problems keeping medical appointments and monitoring their health and 36% felt interpersonal challenges due to their medical issues. 43% of the readmitted patients had problems in 50% of the evaluated BoT domains.
Conclusions: Current healthcare systems and guidelines are not designed to adapt care for the large and growing number of patients with complex care needs. Our findings underline the need for holistic, patient-centered innovative care to improve health and function for patients with heart failure, while addressing social determinants and burden of treatment, as they navigate poorly coordinated healthcare silos which mandate implementation of disease-specific guidelines and care pathways to meet narrowly defined performance measures.