Background: The CDC Core Elements of Antibiotic Stewardship recommend that patients initiated on broad-spectrum antibiotics (BSA) undergo antibiotic de-escalation within 48-72 hours based on available culture data. However, adherence with this recommendation in patients with sepsis has not been well studied. We assessed the incidence of, and characteristics associated with, anti-methicillin resistant staphylococcus aureus (MRSA) and anti-pseudomonas aeruginosa (PSA) antibiotic de-escalation among patients with community-onset sepsis and negative microbiological data across 69 hospitals participating in the Michigan Hospital Medicine Safety Consortium’s sepsis initiative (HMS-Sepsis).
Methods: The HMS-Sepsis registry includes hospitalized patients meeting the CDC surveillance criteria for community-onset sepsis. Patient data, including microbiology results and antibiotic treatment, are entered into the registry by trained, professional abstractors. In this study, we included patients in the HMS-Sepsis registry (discharged 11/8/2020-7/15/2023) who were treated with anti-MRSA or anti-PSA antibiotics on hospital days 1 or 2 and whose laboratory and body fluid culture data through hospital day 3 did not indicate ongoing need for corresponding BSA. De-escalation was defined as discontinuation of anti-MRSA or anti-PSA antibiotics by hospital day 4. Patients remaining on BSA on day 4 were considered a failure to de-escalate. We compared characteristics of patients with vs. without de-escalation and assessed variation in de-escalation across hospitals. We used chi-squared and t-tests for categorical and continuous variables, respectively.
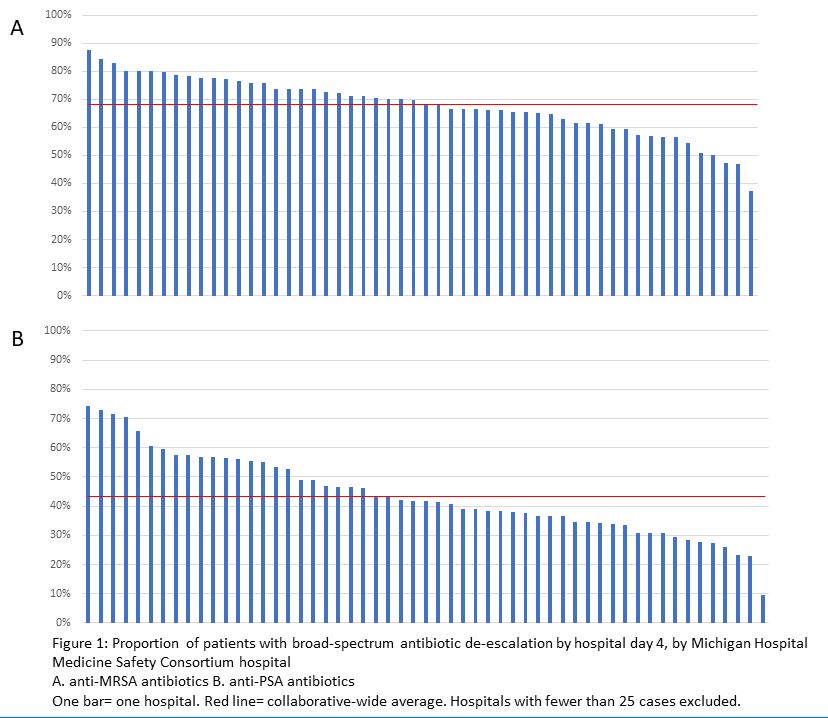
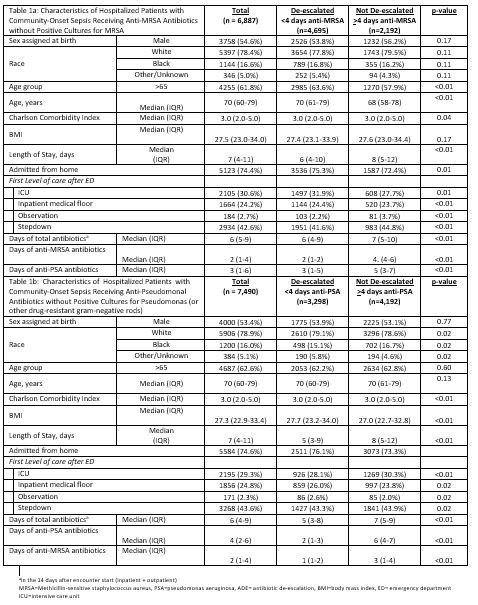
Results: Of 18,169 patients in the HMS-Sepsis registry, 6,887 (37.9%) patients were treated with anti-MRSA and 7,490 (41.2%) were treated with anti-PSA antibiotics and had negative culture data. Of these, 4,695/6,887 (68.2%) with anti-MRSA and 3,298/7,490 (44.0%) with anti-PSA coverage had their antibiotics de-escalated. BSA de-escalation varied by hospital (mean de-escalation of anti-MRSA: 67.8% [range: 37.3-87.5%]; mean de-escalation of anti-PSA: 43.8% [range: 9.7-74.2%], Figure 1). Patients with de-escalation had fewer antibiotic days (empiric anti-MRSA group: median 6.0 [4.0-9.9] vs 7.0 [5.0-10.0], p< 0.01; empiric anti-PSA group 5.0 [3.0-8.0] vs 7.0 [5.0-9.0], p< 0.01) and fewer BSA days (2.0 [1.0-2.0] vs 4.0 [4.0-6.0], p< 0.01; 2.0 [1.0-3.0] vs 6.0 [4.0-7.0], p< 0.01, respectively). De-escalation of anti-MRSA therapy was associated with de-escalation of anti-PSA therapy (and vice versa; Table 1). De-escalation of anti-MRSI occurred in 1,497/2,105 (71.1%) patients admitted to intensive care versus in 1,144/1,664 (68.8%) patients admitted to general care (p=0.12). Meanwhile, de-escalation of anti-PSA occurred in 926/2,195 (42.2%) patients admitted to intensive care versus 859/1,856 (46.3%) admitted to general care (p< 0.01). Unadjusted length of stay was shorter for de-escalated patients (anti-MRSA: median 6.0 [4.0-10.0] vs 8.0 [5.0-12.0) days, p< 0.01; anti-PSA: median 5.0 [3.0-9.0] vs 8.0 [5.0-12.0], p< 0.01).
Conclusions: De-escalation of anti-MRSA and anti-PSA antibiotics occurs in approximately two-thirds and two-fifths of eligible patients with community-onset sepsis, respectively. There is wide variation across hospitals in rates of de-escalation, suggesting an opportunity for practice improvement.