Background: Clostridioides difficile infection (CDI) can be prevented through infection prevention practices and antibiotic stewardship. We found in a 2013 national survey (571 hospitals, 71% response rate) that while infection prevention practices for CDI were common in U.S. hospitals, only 52% had an antibiotic stewardship program (ASP). On 1 January 2017, The Joint Commission required the presence of a multidisciplinary ASP in all U.S. hospitals. The effect of this new mandate on ASP prevalence, especially in smaller hospitals with limited resources, is unknown. We thus conducted a follow-up national survey of U.S. hospitals to determine: a) the presence and composition of ASPs; b) current methods of CDI prevention, treatment, and testing; and c) whether ASP composition and CDI strategies vary by hospital size.
Methods: Surveys were mailed to lead infection preventionists at 900 randomly sampled U.S. hospitals between May and October 2017. Infection preventionists were queried about facility and infection prevention characteristics, including presence of an ASP, ASP team composition, and CDI prevention, treatment, and testing practices. Sampling weights were applied based on the inverse probability of response in each bed size stratum. Responses were compared by hospital bed size using weighted logistic regression.
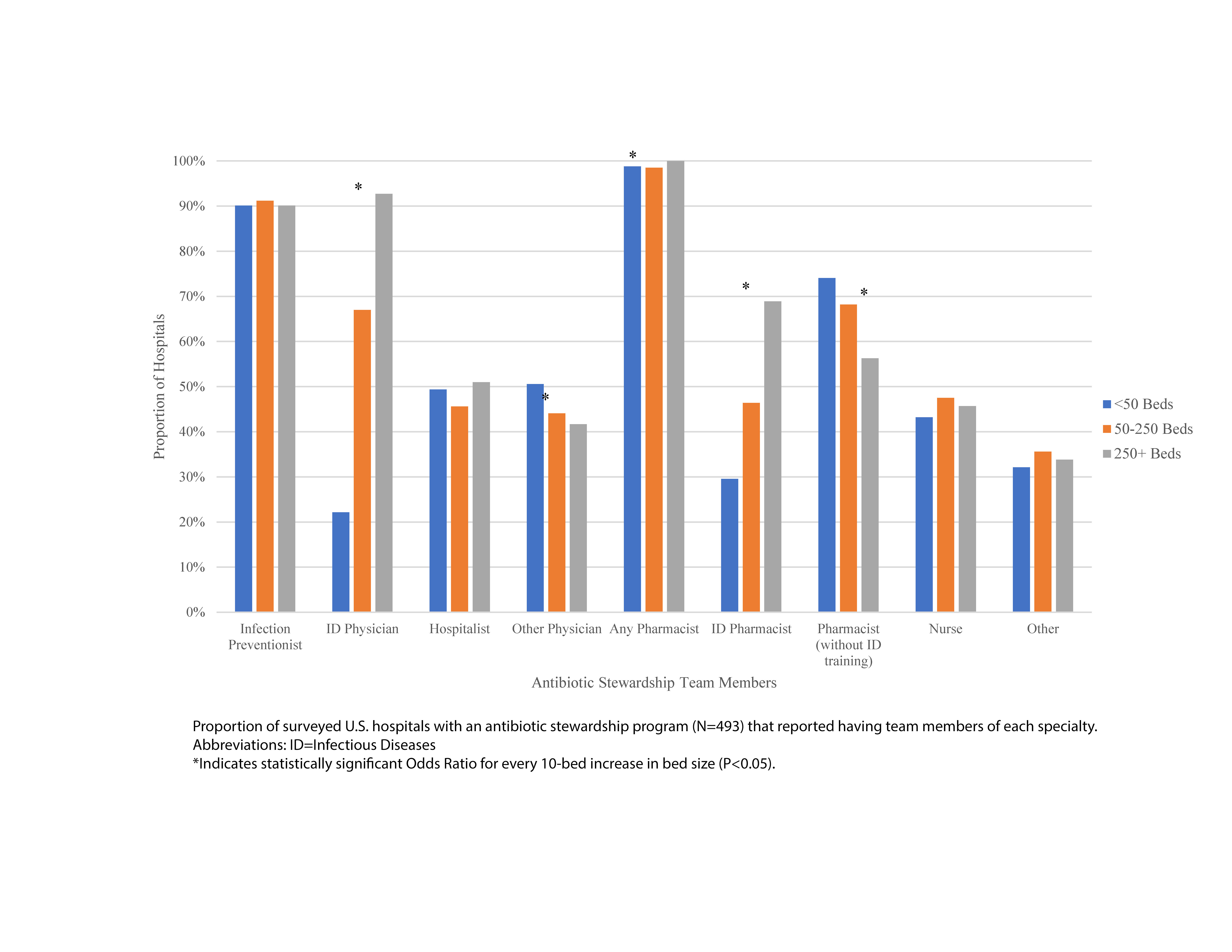
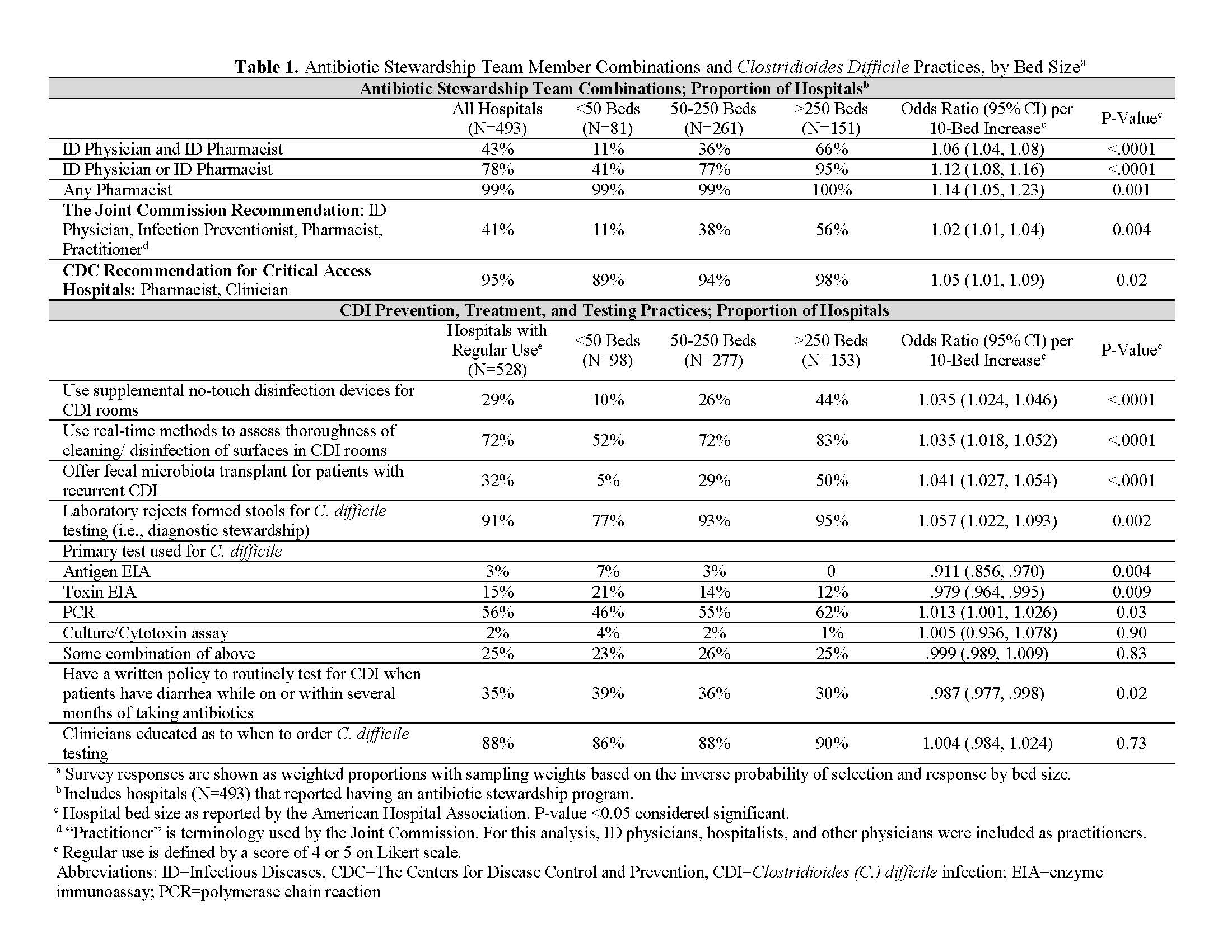
Results: In total, 528 surveys were completed (59% response rate). Though nearly all (95%) hospitals had an ASP, only 41% of hospitals met accreditation standards for multidisciplinary teams (i.e., infectious diseases [ID] physician, infection preventionist, pharmacist, and practitioner). Smaller hospitals were significantly less likely to have stewardship team members with ID training or meet standards for multidisciplinary teams (Table 1). Nearly half of hospitals (46%) had hospitalists involved in stewardship, irrespective of bed size (Figure 1). Guideline-recommended CDI prevention practices were common; however, smaller hospitals were less likely to use high-tech disinfection devices, fecal microbiota transplantation, or diagnostic stewardship strategies (Table 1).
Conclusions: Following changes in accreditation standards, nearly all U.S. hospitals now have an ASP. Many facilities — especially smaller hospitals — still struggle with access to ID expertise and newer CDI prevention, treatment, and testing practices. Given the ubiquity of hospitalists (present in 75% of hospitals and growing), CDI prevention could be enhanced by emphasizing the role of hospitalists in antibiotic stewardship.