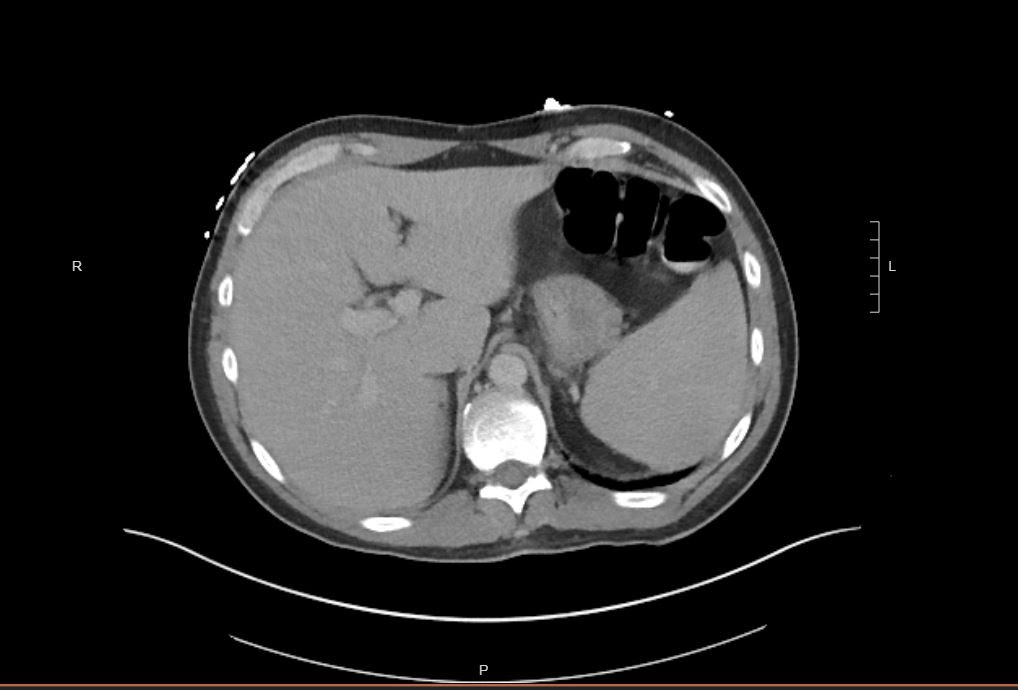
Case Presentation: 42-year-old male with HIV on ART presented in May with six days of fevers, non-bloody diarrhea, headache, and neck pain. He reported dyspnea and dry cough with potential exposure to COVID-19 as he had recently attended local protests. He reported new sexual partners and recently found ticks on himself.He was febrile and tachycardic. He had point tenderness over his thoracic spine and lymphadenopathy in the right axilla. He showed no focal neurological deficits. Labs revealed thrombocytopenia, transaminitis, and hemolytic anemia. COVID-19 PCR was negative.Tick-borne illnesses were evaluated by Babesia, Ehrlichia/Anaplasma, Lyme, and Rocky Mountain Spotted Fever serologies as well as Lyme and Ehrlichia PCR. He was also tested for TB, EBV, syphilis, c. difficile, ova and parasites, giardia, norovirus, gonorrhea, and chlamydia.CT Head was negative for acute abnormalities. CT Abdomen/Pelvis showed hepatosplenomegaly. Lumbar puncture was negative for meningitis. EGD found non-specific discoloration of esophageal mucosa and gastric erosions for which random biopsies were taken. Pathology was unremarkable. Colonoscopy was unrevealing.After four days, results showed E. Chaffeensis IgG 1:1024, IgM undetectable, and E. Chaffeensis by PCR abnormal/detected. HIV RNA was positive. His symptoms resolved after initiating doxycycline.
Discussion: When evaluating febrile diarrhea in an HIV patient, it is important to determine immune status and acuity. If HIV has not progressed to AIDS, the differential is similar to that of an immunocompetent patient. Acute presentations raise concern for bacterial and viral etiologies. Ehrlichosis is a rare tick-borne illness caused by E. Chafeensis and E. Ewingii transmitted by the lonestar tick, commonly found in the Southeastern United States. Symptoms are non-specific, including fever and malaise. Severe disease can result in multi-organ system failure.HIV-positive patients are at similar risk for developing ehrlichiosis as healthy individuals, though their disease presentation is more severe.Ehrlichiosis has strong associations with geography and seasonality. The white-tailed deer is the main vector, and dogs are also known to transmit disease. Fever can be the presenting symptom in an HIV-infected patient, and 10% of all ehrlichiosis patients have diarrhea.The unique confluence of the COVID-19 pandemic and possibility for increased disease transmission from non-socially distanced activities such as protests, raised concern for COVID in our patient. Diarrhea has been reported in 11% of patients. Patients with AIDS are at risk for opportunistic infections that cause diarrhea. C. difficile should be considered in all patients with HIV, which alters the intestinal microbiome. High-risk sexual practice is a risk factor for HSV, neisseria, chlamydia, giardia, and entamoeba diarrhea. Considering our patient’s fever, immunocompetent status and acuity of diarrhea, infectious etiology remained at the top of the differential. Labs and imaging often reveal pancytopenia, transaminitis, and hepatosplenomegaly. Presence of E. chaffeensis antibodies is diagnostic and PCR can confirm infection. Diagnostic tests can take days to result.
Conclusions: Ehrlichiosis should be considered in all patients with HIV presenting with febrile diarrhea in endemic areas. If suspicion is high, empiric tetracycline therapy should be started immediately, as ehrlichiosis is more severe and possibly fatal in the HIV population.