Background: Infants ≤ 60 days of age with a urinary tract infection (UTI) are a challenging population. Without clear guidelines for management, there is variability in renal imaging and antibiotic use. Our study examined patterns of renal imaging and antibiotic use in infants ≤ 60 days of age with UTI at a tertiary care children’s hospital.
Methods: We identified infants age ≤ 60 days of age hospitalized from 1/2013 – 1/2017 using diagnostic codes for UTI or fever. Inclusion criteria were urine culture obtained, renal imaging obtained, and final diagnosis of UTI. Exclusion criteria were treatment of a separate source of infection, comorbid conditions, prior genitourinary manipulation within 7 days, and hospital-acquired UTI. The primary outcome was inpatient renal ultrasound (RUS) evaluation. Secondary outcome was follow-up RUS or voiding cystourethrogram (VCUG). RUS abnormalities were classified as “insignificant abnormality” if mild pelviectasis or pyelonephritis were present in isolation and “significant abnormality” if moderate/severe pelviectasis or other anatomic abnormality was identified. RUS results were confirmed by an independent radiologist. We measured the association of abnormal RUS with timing of inpatient RUS, presence of bacteremia, presence of atypical pathogen, ill appearance, and antibiotic prophylaxis, using Chi-square and Fisher’s exact tests. Data are reported as numbers and proportions.
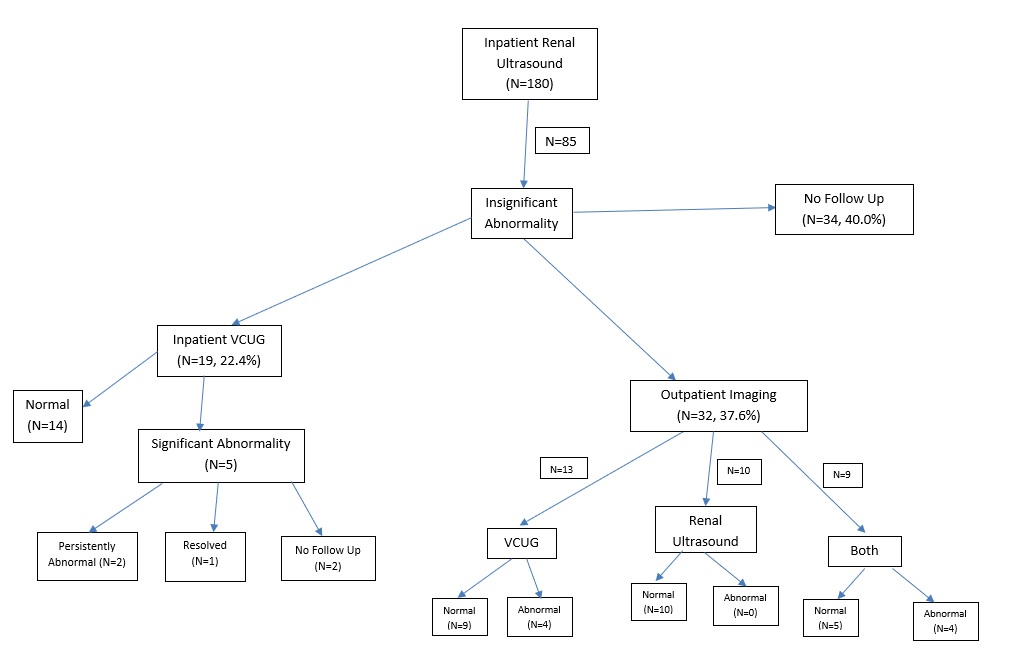
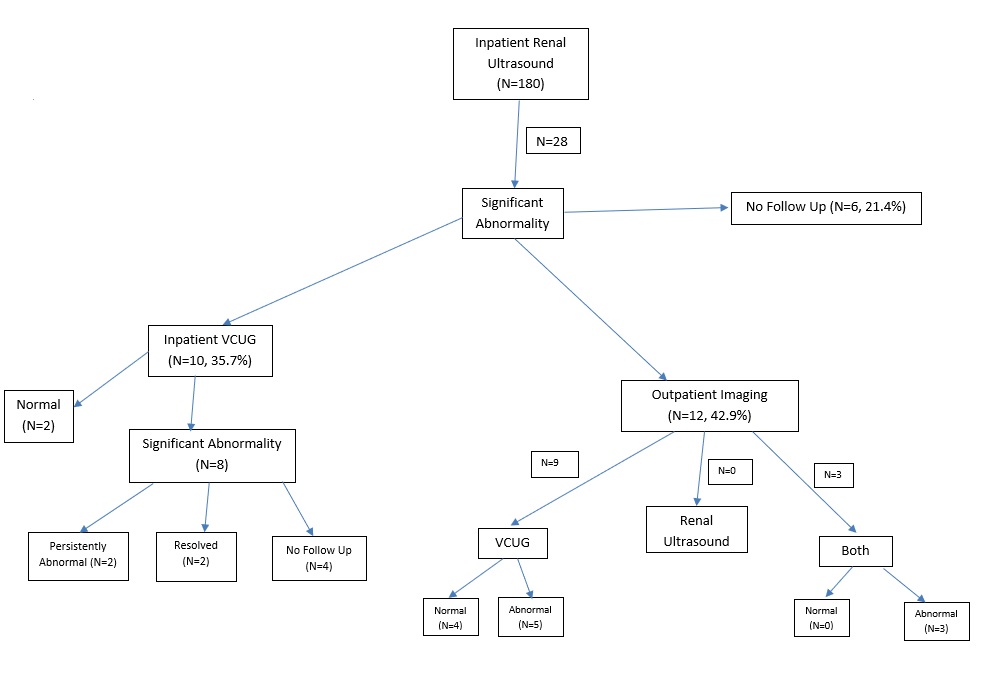
Results: 187 infants met inclusion criteria. 180 (96.3%) had inpatient RUS , of whom 36 (20%) also had inpatient VCUG. The remaining 7 had only outpatient imaging. Of inpatient RUS, 67 (37.2%) were normal, 85 (47.2%) had insignificant abnormality, and 28 (15.6%) had significant abnormality. Of 85 infants with insignificant abnormality on inpatient RUS, 19 (22.4%) had inpatient VCUG, 32 (37.6%) had further outpatient imaging, and 34 (40.0%) had no follow up; overall, 13/85 infants (15.3%) had an abnormal urinary tract on follow-up. Of 28 infants with significant abnormality on inpatient RUS, 10 (35.7%) had inpatient VCUG, 12 (42.9%) had outpatient imaging, and 6 (21.4%) had no follow up; overall 16/28 infants (57.1%) had an abnormal urinary tract on follow-up. 42/180 (23.3%) of infants were started on antibiotic prophylaxis before discharge. Of these, 7 (16.7%) had no abnormality, 16 (38.0%) had insignificant abnormality, and 19 (45.2%) had significant abnormality on inpatient RUS. 11 infants (26.2%) initiating antibiotic prophylaxis had no urinary tract abnormalities on any evaluation. Infants with fever >48 hours were significantly more likely to have abnormal imaging (p=0.032). Presence of bacteremia and an atypical pathogen showed a trend toward association with imaging abnormality.
Conclusions: In this retrospective study of young hospitalized infants with UTI, the large majority had inpatient imaging. Though about half showed insignificant abnormalities, many had further imaging, perhaps unnecessarily. Nearly one-quarter of infants were started on antibiotic prophylaxis, although more than half of these did not have significant abnormalities on initial imaging and more than a quarter ultimately had normal urinary imaging. Outpatient follow-up on abnormalities was poor. A standardized approach to renal imaging and interpretation in young infants with UTI may decrease unnecessary follow-up imaging and prophylactic antibiotic exposure.