Background: Midlines are peripheral vascular devices inserted in the veins of the upper extremity with the tip located at or below the axillary vein. Complications associated with peripherally inserted central catheter (PICC) along with documented overuse has led to emerging interest and increasing use of midlines. However, whether midlines are safer than PICCs is not known.
Methods: Trained abstractors collected data on a representative sample of PICC and midline placements at 48 hospitals participating in the Michigan Hospital Medicine Safety (HMS) consortium between January 2014 and August 2018. Patients were followed until PICC or midline removal, death or 30 days post-placement. We compared PICCs and midlines placed for difficult intravenous access, frequent phlebotomy or antibiotics with respect to device characteristics, dwell time and incidence of complications. Major complications included upper extremity deep vein thrombosis (DVT), catheter-related blood stream infection (BSI), pulmonary embolism, device removal for suspected blood stream infection (BSI) and catheter occlusion. Minor complications were defined as accidental dislodgement, tip migration, exit site infection and superficial thrombophlebitis. Comparisons utilized Chi-Square test and Fisher’s exact test, where appropriate.
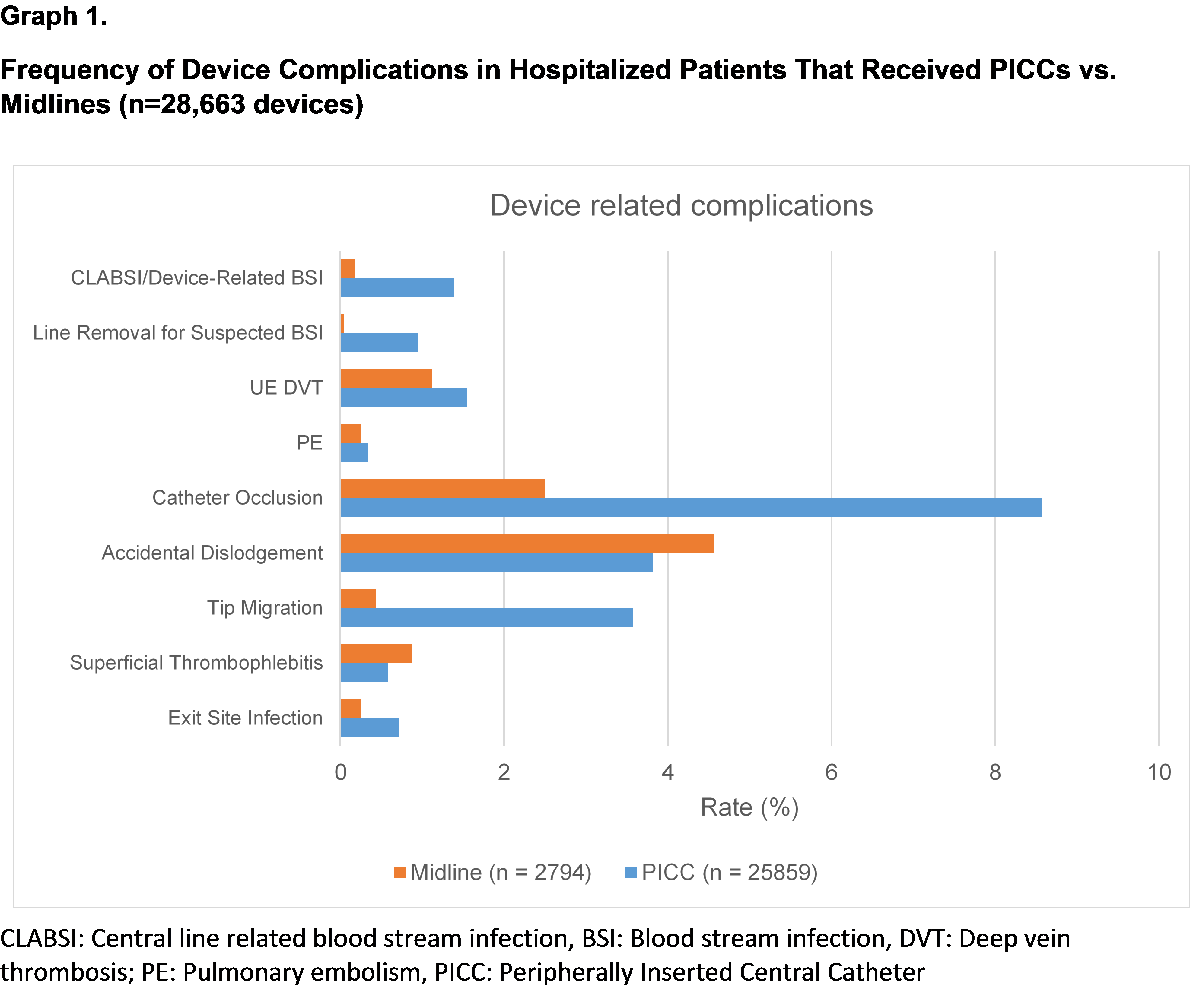
Results: Data on 25,859 PICCs and 2,764 midlines was available for analysis. The average Charlson co-morbidity index and LOS for patients with PICCs was 3.6 and 9.2 days compared to 3.7 and 8.3 days for patients with midlines. Single lumen devices represented 57% (14,735) of PICCs and (1,563) midlines. The average PICC dwell time was 17.13 days (n=20,108); 43% (8,562) of PICCs remained in place greater than 15 days after placement. In contrast, the average dwell time for midlines was 7.1 days (n=2,331); only 11% (254) of midlines remained in place 15 days after placement. Major complications occurred in 11% (2,888) of PICCs versus 4% (111) of midlines. The most common PICC complication was catheter occlusion (8.6%), which was infrequent in midlines (2.5%). A total of 245 PICCs (0.95%) were removed for a suspected BSI; in contrast, only 1 midline (0.04%) was removed for this reason. Minor complications occurred in 8% (2,014) of PICCs vs. 5.8% (161) of midlines, with a trend towards more accidental dislodgements and superficial thrombophlebitis noted in midlines. Notably, 30% (7,646) of patients with PICC had an ER visit or hospital re-admission within 30 days of placement, compared to 12% (339) of patients with midlines, (P<0.001 for all outcome comparisons) (Figure 1).
Conclusions: From the perspective of complications and patient-centered outcomes, midlines appear to be safer than PICCs, and may have an important role in vascular access for select hospitalized patients.