Case Presentation: The patient, a 29-year-old G1P1 female, presented to the emergency department with a 3-day history of double vision, frontal headache, and gait instability. Eye examination was significant for asymmetric bilateral internuclear ophthalmoplegia. Admission labs demonstrated mild leukocytosis without left shift and elevated inflammatory markers including complement levels and IL-6. An MRI of the spine and head revealed no evidence of demyelinating illness. Upon further review of the history, it was noted that the patient had an upper respiratory illness 3-weeks ago, followed by neck stiffness and cold sores which resolved spontaneously without treatment. A lumbar puncture was ordered; however, the patient was empirically given Acyclovir before it could be obtained and her symptoms improved significantly. Later, CSF studies showed lymphocytic pleocytosis with normal protein levels suggesting aseptic meningitis, however, CSF and serum PCR were negative for common viral pathogens including HSV and VZV. Multiple sclerosis workup came back negative, and she was discharged on oral valacyclovir 1 gram three times daily for two weeks.
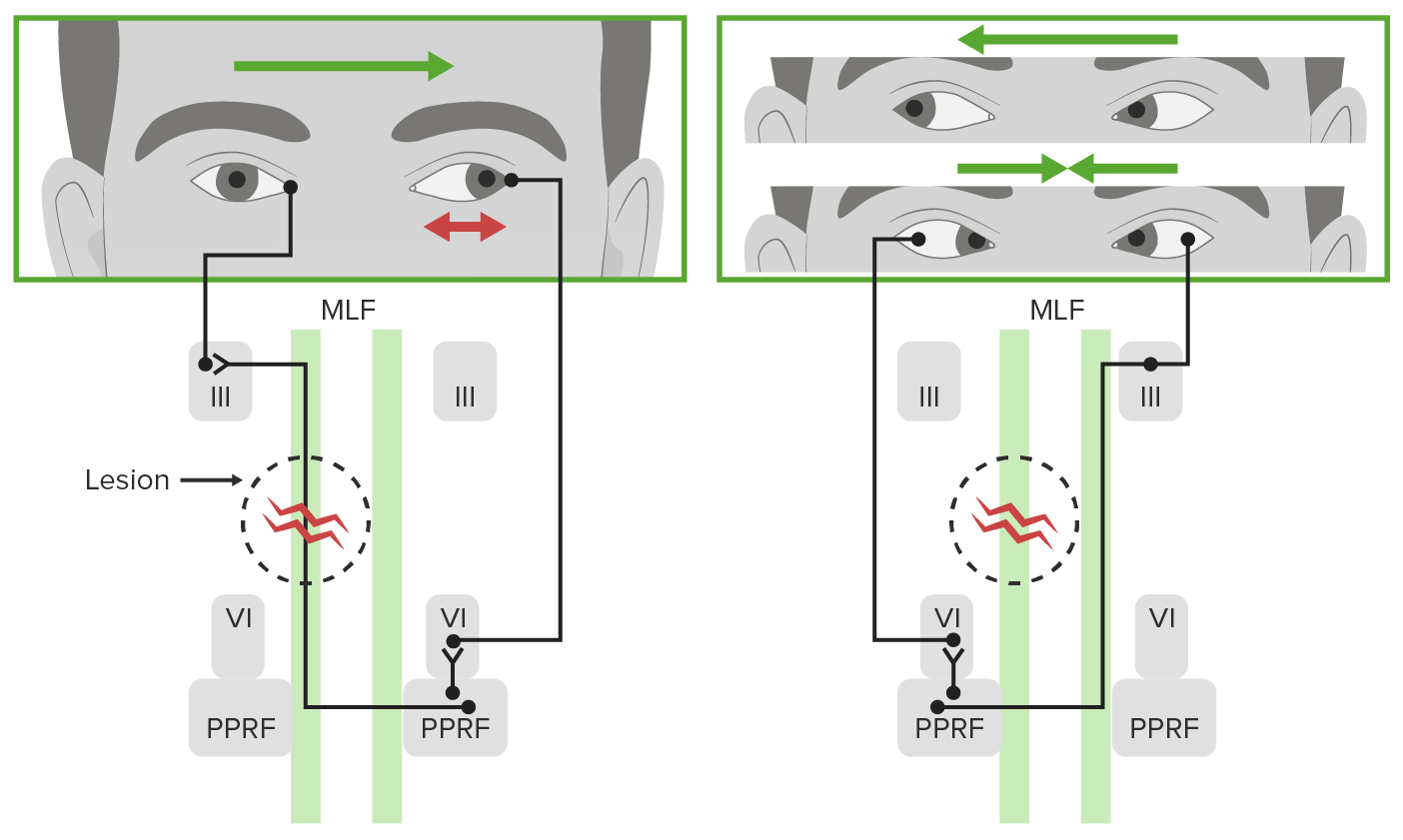
Discussion: Internuclear Ophthalmoplegia (INO) is caused by damage to a heavily myelinated bundle of neurons called Medial Longitudinal Fasciculus, which connects the nucleus of ipsilateral cranial nerve III with the nucleus of contralateral cranial nerve VI. It is characterized by the inability to adduct the eye on the affected side, coupled with impaired abduction of the contralateral eye. The typical presentation includes nystagmus, horizontal diplopia, dizziness, gait instability, and headaches. Although imaging including, MRI and proton density imaging can help visualize lesions, INO is a clinical diagnosis. CSF analysis is reserved for cases where infection or Multiple Sclerosis is strongly suspected. Treatment involves the management of the underlying cause. Demyelinating disorders, particularly Multiple Sclerosis, are the most common cause of INO. Less frequent causes include brainstem infarctions, hemorrhage, trauma, vasculitis, and bacterial, or viral infections. Bilateral INO is particularly significant as it is strongly suggestive of Multiple Sclerosis and warrants complete workup for Multiple Sclerosis. Although less prevalent than other causes, aseptic meningitis should be in the differential as preceding infections can be very subtle. In these instances, diagnosis is made with the help of CSF analysis, cultures, and PCR. However, it is important to remember that CSF is sterile in the majority of cases, especially if patients have already received antimicrobials.
Conclusions: Although less prevalent than other causes, aseptic meningitis should be in the differential in patients presenting with Bilateral Internuclear Ophthalmoplegia as preceding infections can be very subtle. In these instances, diagnosis is made with the help of CSF analysis, cultures, and PCR. However, it is important to remember that CSF is sterile in the majority of cases, especially if patients have already received antimicrobials.