Background:
Increasing hospital efficiency has resulted in lower hospital length of stay (LOS); however, the impact of reduced LOS and hospital readmission rates has not been well described. Our objective was to determine trends in hospital LOS and 15‐day read‐mission rates for all medical diagnoses and 4 common diagnoses over 10 years in the Veterans Administration (VA), the largest single provider of health care in the United States.
Methods:
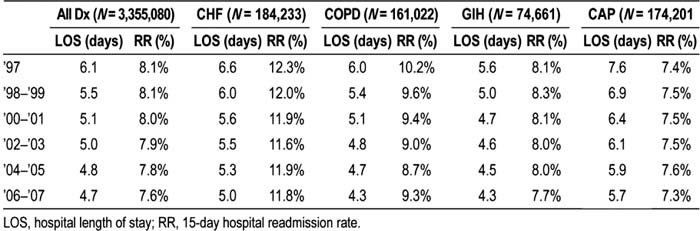
The study sample included 3,655,080 medical admissions to 129 VA hospitals from 1997 to 2007, with subsamples of patients with 2 chronic conditions [congestive heart failure (CHF; N = 184,233) and chronic obstructive pulmonary disease (COPD; N = 161,022)] and 2 acute conditions [community‐acquired pneumonia (CAP; N = 174,201) and gastrointestinal hemorrhage (GIH; N = 74,661)]. Exclusions included in‐hospital death, transfers to other hospitals, and LOS > 30 days. Unadjusted LOS and 15‐day readmission rates were determined in 2‐year increments with 1997 as the baseline year.
Results:
For all diagnoses from 1997 to 2007, mean hospital LOS decreased from 6.1 to 4.7 days. During the same interval, 15‐day readmission rates also were reduced, from 8.1% to 7.6%. For individual diagnoses, LOS reductions were observed for the 2 chronic conditions, CHF (from 6.6 to 5.0 days) and COPD (from 6.0 to 4.3 days), and the 2 acute conditions, GIH (from 5.6 to 4.3 days) and CAP (from 7.6 to 5.7 days). Over the same 10‐year period, 15‐day readmission rates decreased for CHF (from 12.3% to 11.8%), COPD (from 10.2% to 8.3%), and GIH (from 8.1 % to 7.7%), but not for CAP (from 7.4% to 7.3%).
Conclusions:
VA hospitals demonstrated significant improvements in inpatient efficiency over the past 10 years, with a 23% relative reduction in LOS and a concomitant 6% relative reduction in hospital readmissions during the same time interval. LOS reductions were similar across all 4 high‐volume diagnoses, and 15‐day readmission reductions were similar for 3 of 4. These findings suggest that as efficiency has improved, it has not been at the cost of increased hospital readmission. This is particularly important, as hospital readmission is considered a quality indicator and may result in payment denial for hospitals. Future work should explore these relationships at a hospital level to see if a tipping point exists for LOS reduction and hospital readmission.
Author Disclosure:
J. Go, none; M. Vaughan‐Sarrazin, none; P. Kaboli, none.