Background: Syncope is usually an isolated occurrence in younger patients whereas it is multi factorial with many predisposing factors in the elderly. Medication use, co-morbidities and functional decline further complicate syncope evaluation in the elderly. Hence, elderly patients presenting with syncope must be risk stratified uniquely. San Francisco Syncope Rule (SFSR) and Evaluation of Guidelines in Syncope Study (EGSYS) are two widely validated syncope evaluation scores, but never had a head to head comparison in the geriatric population. Objective of our study was to compare these two scoring systems in predicting composite adverse outcome (cardiovascular events, pulmonary embolism, bleeding, death) at 48 hours and 30-days.
Methods: In this single center retrospective cohort study, we evaluated patients of age 65 or above who presented to a large academic center with syncope, during the period of 01/01/2017 to 12/31/2018. Patients with confirmed non-syncopal syndromes, active acute medical condition, drug or alcohol use prior to the event were excluded from the study. Patients were risk stratified into high risk and low risk based on both SFSR and EGSYS scores independently. Composite outcome analysis were based on adverse event within 48 hours and 30-days of the syncopal event which included death, myocardial infarction, arrhythmia, arrythmogenic condition, new diagnosis of structural heart disease, pulmonary embolism, stroke, serious hemorrhage or any condition causing a return ED visit/hospitalization/ procedural intervention. Data quality was assessed to minimize inter-observer variability using a representative sample from the cohort. Demographic, clinical characteristics and prevalence of adverse events were calculated among EGSYS and SFSR risk categories. Least squared means and likelihood ratio were used to find significant difference across the categories for continuous and categorical variables respectively. A multivariate adjusted logistic regression model was used to predict adverse outcome by high risk score categories in reference to low risk score groups separately in two different scoring system.
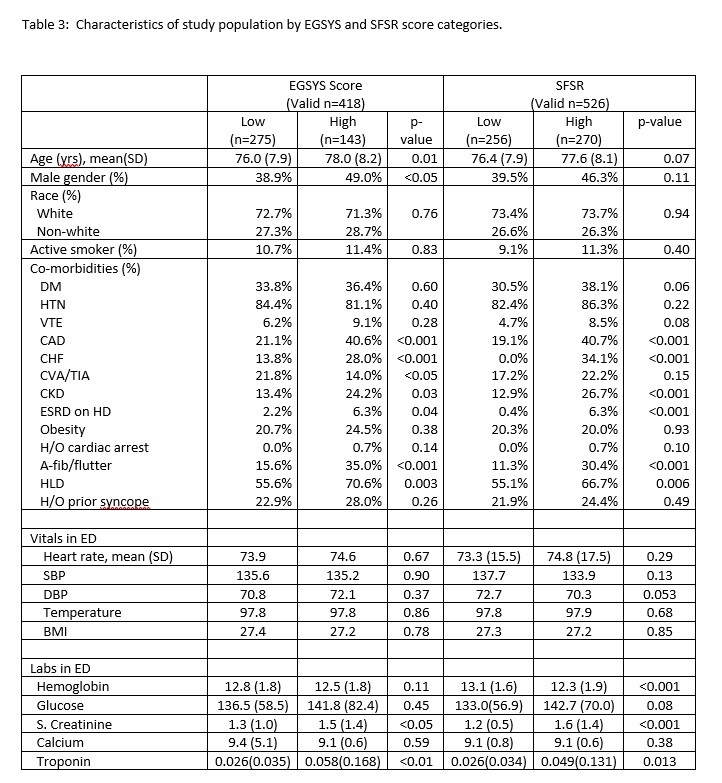
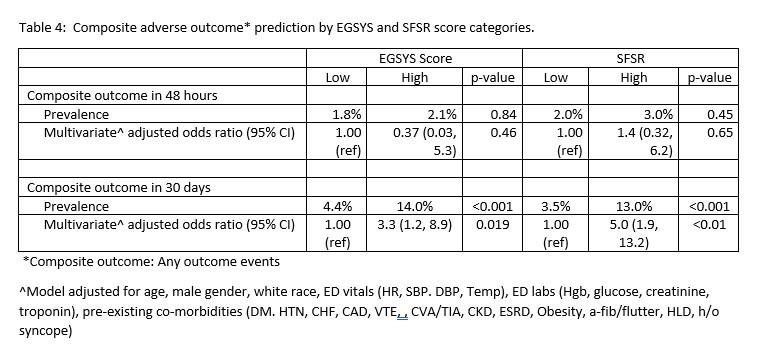
Results: Among 548 eligible study population, EGSYS and SFSR score could be calculated in 418 and 526 patients respectively. Prevalence of high risk EGSYS and SFSR scores were 34.2% and 51.3% respectively. High Risk EGSYS score group was older (mean age 78.0 years) and had male predominance (49%) compared to low EGSYS score group. No such difference was present among SFSR groups. Prevalence of smokers, co-morbidities, emergency department vitals and labs were very comparable with small differences in certain variable among two groups within each system. Statistically non-significant but higher trend of 48 hours adverse outcome were noted in high risk groups. Prevalence of 30-days adverse outcome was significantly higher among high risk group (EGSYS: 14%, SFSR 13%) compared to low risk groups (EGSY: 4.4%, SFSR: 3.5%). Multivariate adjusted odds ratio of 30-days adverse outcome among high risk group was 3.3 (95% CI: 1.2, 8.9) in EGSYS and 5.0 (1.9, 13.2) in SFSR in reference to respective low risk group.
Conclusions: In the same geriatric population prevalence of high-risk score was lower using EGSYS method than SFSR method. Statistically significant odds ratio is associated with high risk group in both methods, but strength of association is greater using SFSR method. Difference in categorizing high risk syncope groups exits between different syncope scoring methods.