Background: Patient- and family- centered care (PFCC) is a key element of safe healthcare. Family-centered-rounds (FCR) incorporate PFCC into the daily workflow of children’s hospitals. This observational study assessed whether our rounds on the Baystate Children’s Hospital Infant’s and Children’s unit met key goals of FCR including providing medical information, engaging in open, bidirectional communication, and showing empathy.
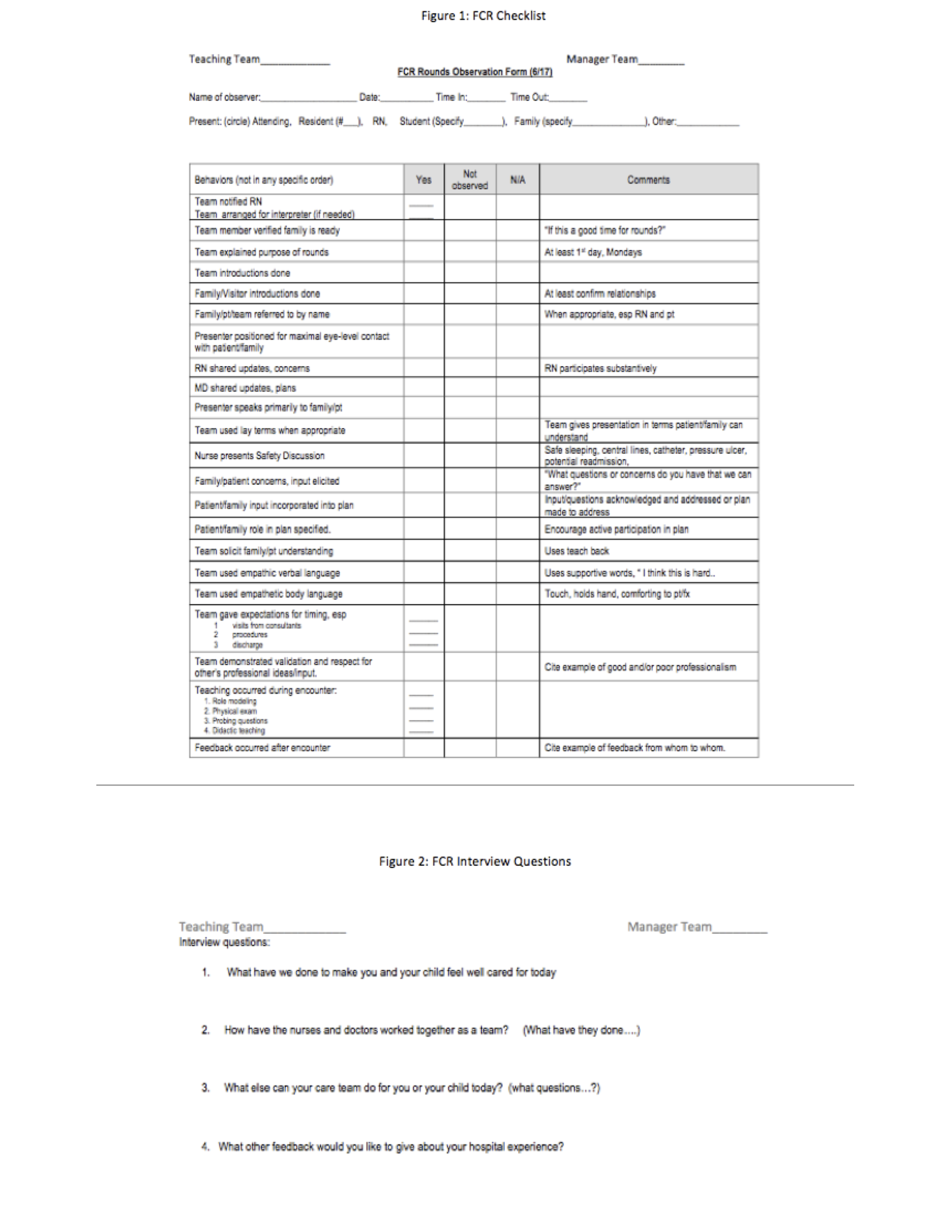
Methods: We reviewed literature on FCR practices and developed a checklist evaluating specific behaviors (Figure 1 and Figure 2) during FCR on our academic pediatric inpatient unit. Trained non-physician observers completed the checklist on rounds. After rounds, the observer interviewed the patient and family for additional perspectives on their care. Inclusion criteria were family willingness to participate, presence in room, and English language proficiency or interpreter availability. Residents and nurses learned FCR principles during scheduled educational sessions. Families were informed of FCR on admission. Observations occurred from 5/2017 to 10/2017. Data were entered into REDCap.
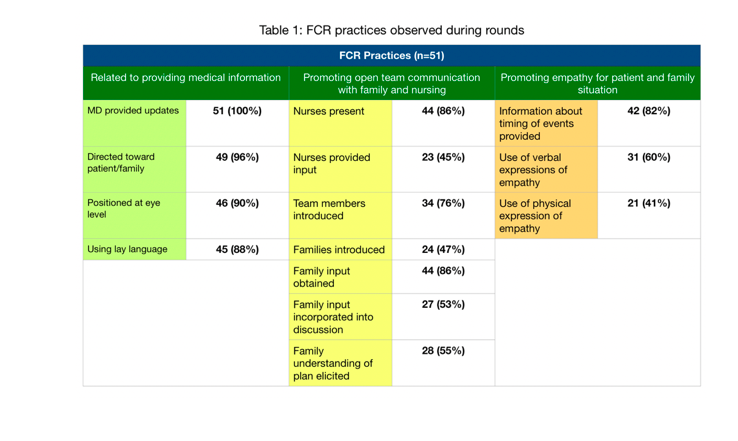
Results: 54 observations were completed; 3 were excluded due to absence of family/ patient. 12 were interviewed. The observations and interviews identified three themes pertinent to FCR: provision of medical information, demonstration of open team communication, and demonstration of empathy for the patient and family (Table 1). Practices related to providing medical information occurred in most encounters. With respect to open team communication, nurses were present in 44 (86%) and nursing input was obtained in 23 (45%) of observations. Family input was obtained in 44 (86%) of encounters and family input was incorporated into plan and their understanding of the plan was observed in 27 (53%) and 28 (55%) encounters respectively. Empathy was expressed verbally by the team in 31 (60%) and physically in 21 (41%) of observations. Positive interview comments correlated with areas of higher adherence to FCR principles during rounds; negative comments correlated with lower adherence.
Conclusions: Following the basic components of FCR, such as having teams meet in the room with the nurse, patient and family and using family centered language, does not always lead to shared decision making and open communication between rounding teams, nurses, and patients, and does not necessarily foster empathic relationships. Our next steps will focus on improving the use of FCR to role model and develop a culture of open communication, shared decision making and empathy.