Background: Behavioral emergencies in the hospital are on the rise, leading to increased workplace violence. A small body of evidence recommends an inpatient Behavioral Emergency Response Team (BERT), a multi-disciplinary team to de-escalate behavioral emergencies that can be harmful to the patient or staff. Observational studies have reported that BERT can reduce workplace violence, use of restraints, and security calls. We sought to assess the efficacy of the BERT our institution, specifically evaluating nursing concerns and comparing nursing and BERT viewpoints on behavioral emergencies, to identify areas for improvement in safety.
Methods: A 7-question survey was developed to assess nursing views on management of behavioral health emergencies and suspected root causes for these events. This survey was administered to the primary or charge nurse involved in events requiring BERT assessment from March 2022 to May 2023 at a 900-bed academic safety-net hospital. BERT staff were already required to complete a documented template for the electronic medical record with analogous questions. 39 points of comparison were obtained.
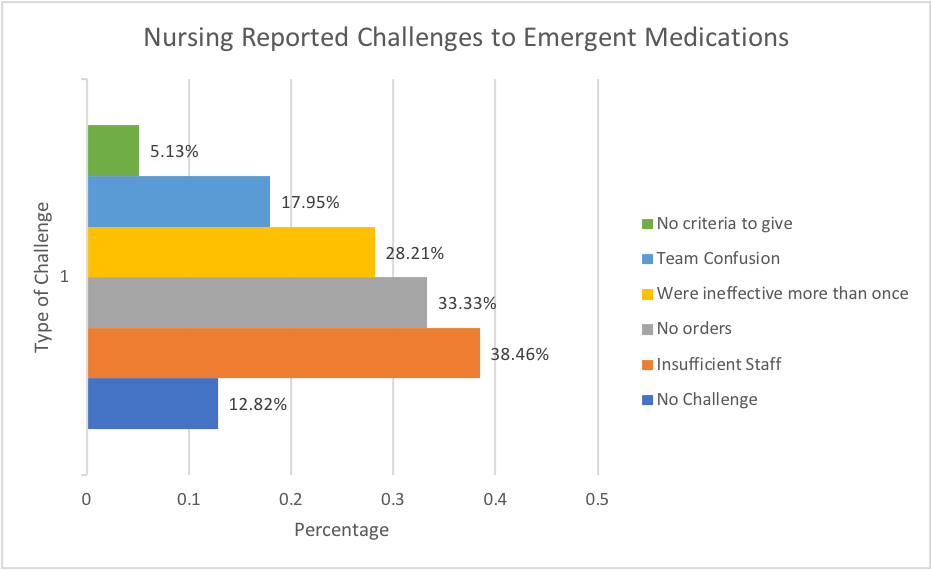
Results: A total of 46 surveys were completed after BERT evaluations out of a total estimated 800 BERT calls over the study period. 49% of nurses reported no challenges with placing restraints and 13% had no challenges administering agitation pro re nata (PRN) medications. The most common challenges to administering PRN medications included perception of insufficient staffing (38%), reported lack of PRN med orders (33%), PRNs had already been ineffective previously (28%), and inadequate role clarification amongst the team (17%). Preceding BERT activation, 87% of nursing staff used verbal de-escalation, and 56% used PRNs for anxiety or pain. Nursing staff and BERT staff felt that the primary etiology for the behavioral emergency differed 51% of the time. BERT primary intervention included verbal de-escalation (23%) and IM or PO agitation medication (60%). BERT secondary intervention included verbal de-escalation (38%).
Conclusions: During behavioral emergencies, the majority of nursing respondents reported difficulty with administering agitation medications, reporting perceived insufficient staffing as one of the primary challenges. While nursing staff utilized verbal de-escalation in most situations, BERT utilized verbal de-escalation as a core strategy in half of behavioral emergencies including as the primary strategy one quarter of the time, suggesting BERT may be more successful with verbal de-escalation strategies for a subset of these patients. This may indicate an area for improvement in exact verbal de-escalation techniques used by nursing. BERT teams strive to fill these gaps. Next steps include piloting new nurse simulation lab training for behavioral health emergencies to enhance skills of verbal de-escalation, restraint use, and PRN medication use. Protocols for earlier psychiatry consultation in high-risk patients may also ensure PRN medications are ordered in a timelier manner. Future directions could evaluate whether better nursing preparedness in behavioral health emergencies could improve nursing morale, engagement and retention.