Background: There is a population of patients who visit Emergency Department (ED) frequently and this has become a challenge for the health-care system. A small proportion, four percent of ED patients, could constitute up to 20% of ED visits (1-3).Interdisciplinary approach of care management is the most widely evaluated and single-point-of contact (4).We conducted a Quality Improvement (QI) project in our Internal Medicine (IM) residency clinic, to investigate if scheduling the same PCP resident for each outpatient visit, improving patient outreach, and easier access to the PCP resident would reduce the number of ED visits and hospitalizations.
Methods: Our QI project, consisted of three residents. We identified 100 patients from our IM center with three or more ED visits or hospitalizations, between August 2021-August 2022. We started our QI with nine patients. We ensured that during all office visits the QI supervising attending was the preceptor. Enrollment was defined as having an initial office visit with the assigned QI PCP resident.We looked at the number of office visits, ED visits, and hospitalizations as our primary outcomes, average systolic (SBP) and diastolic blood (DBP) pressure over last 3 office visits, hemoglobin A1c, LDL, and completed components preventive measure as our secondary outcomes, one year prior and one year after the enrollment.
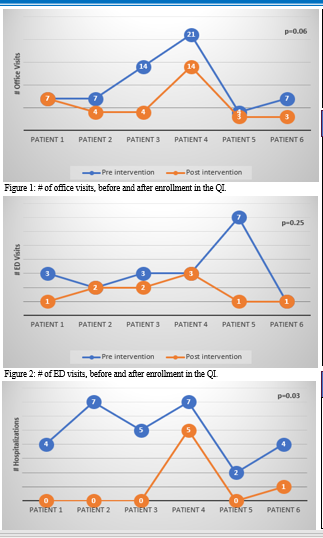
Results: All nine patients were enrolled between August 2022-January 2023. After enrollment, one patient changed their PCP, one was admitted to a long-term to nursing home, and one did not show up after the initial enrollment, excluded from our analysis. We remained with six patients, with mean age of 64 years, 50% male, 67% Caucasian and 33% African-American. After enrollment, 5/6 patients (83%) had decreased office visits, 1/6 (17%) had no change in number of office visits (p=0.06); 3/6 patients (50%) had decreased ED visits, 3/6 (50%) had no change in number of ED visits (p=0.25); 6/6 (100%) had decreased hospitalizations (p=0.03). After enrollment, average SBP decreased in 3/6 (50%), and increased in 3/6 (50%) patients (p=0.41); average DBP decreased in 4/6 (67%) and increased in 2/6 (33%) patients (p=0.31). We assumed a non-normal distribution for our primary and secondary outcomes and used Wilcoxon signed-rank test. After enrollment, not all patients had repeat hemoglobin A1c and LDL, therefore we excluded these values from our analysis. There were no significant changes in completed components preventive measures.
Conclusions: Our QI demonstrates fewer hospitalizations with improvement and optimization of continuity of care, both clinically and statically significant. This QI mphasizes importance of PCP residents seeing their patient for each visit. Our sample size is small, but we believe the results are highly significant and we will expand to a large sample size. Improvement of continuity of care translates into better care and decreased healthcare costs.