Background: Availability of acute medical services (e.g., emergency department, intensive care unit) has been associated with adverse clinical outcomes. The association between acute psychiatric inpatient beds and suicide has not been well described. In the Veterans Health Administration (VHA), suicide rates among veterans have increased despite mental health care investments. Our objective was to examine the relationship between veteran suicide risk and availability of acute inpatient psychiatric beds and other community and patient-level factors.
Methods: Veterans enrolled in VHA primary care between 2003 and 2016 were included in this retrospective cohort study using VHA administrative data and publicly available sources for contextual community factors. Data sources included the VHA Clinical Data Warehouse (patient-level factors), VHA Support Service Center (VHA inpatient psychiatric beds and occupancy rates), Area Health Resources Files (civilian inpatient psychiatric beds), State Mental Health Agency (county-level data on mental health spending), and the National Death Index Suicide Registry. Community-level analyses, including the hospital and surrounding area, were conducted using generalized linear mixed models with random intercepts for hospital, modeling number of suicides per quarter. VHA Bed availability was categorized into quintiles from lowest to highest occupancy.
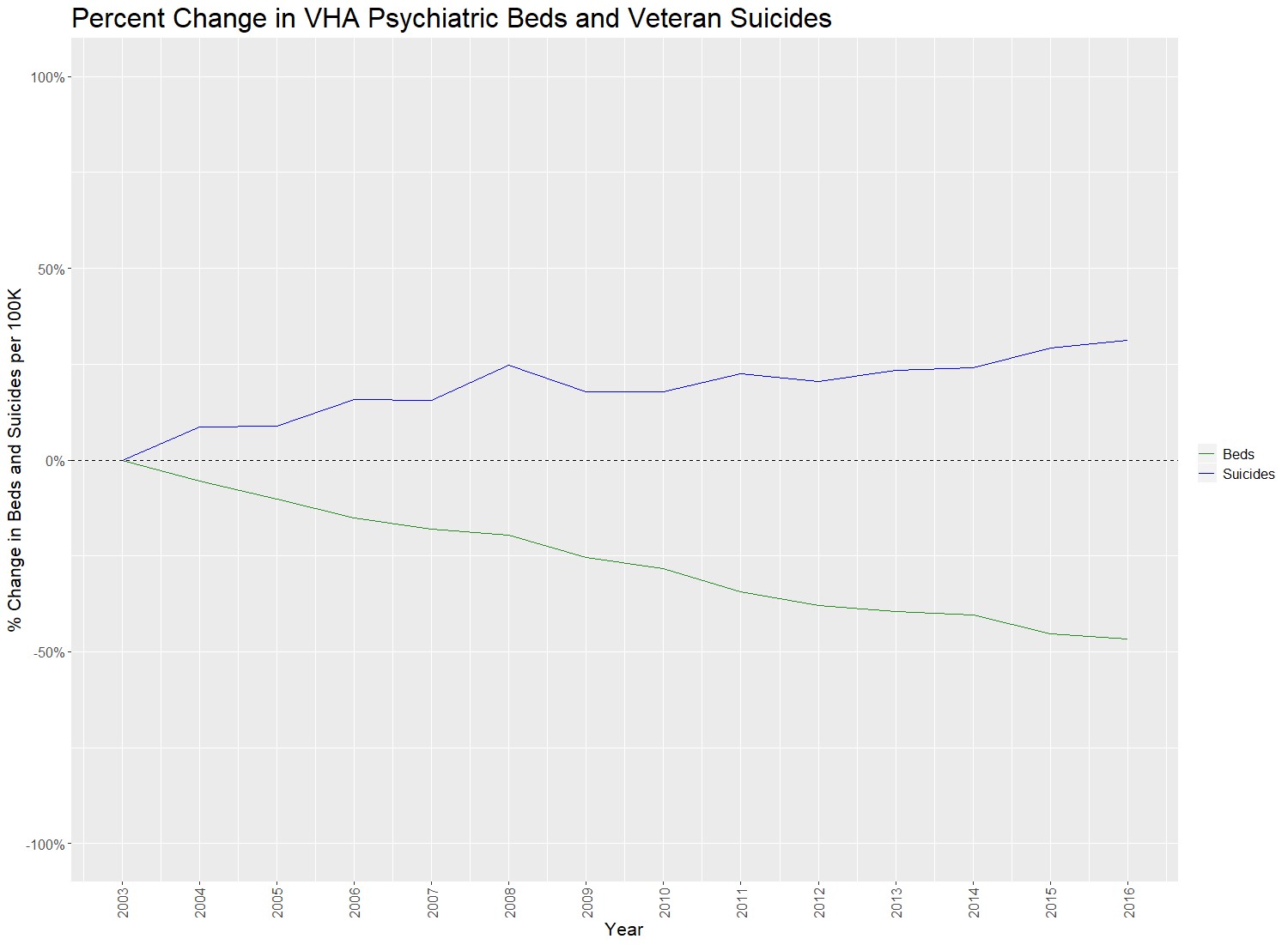
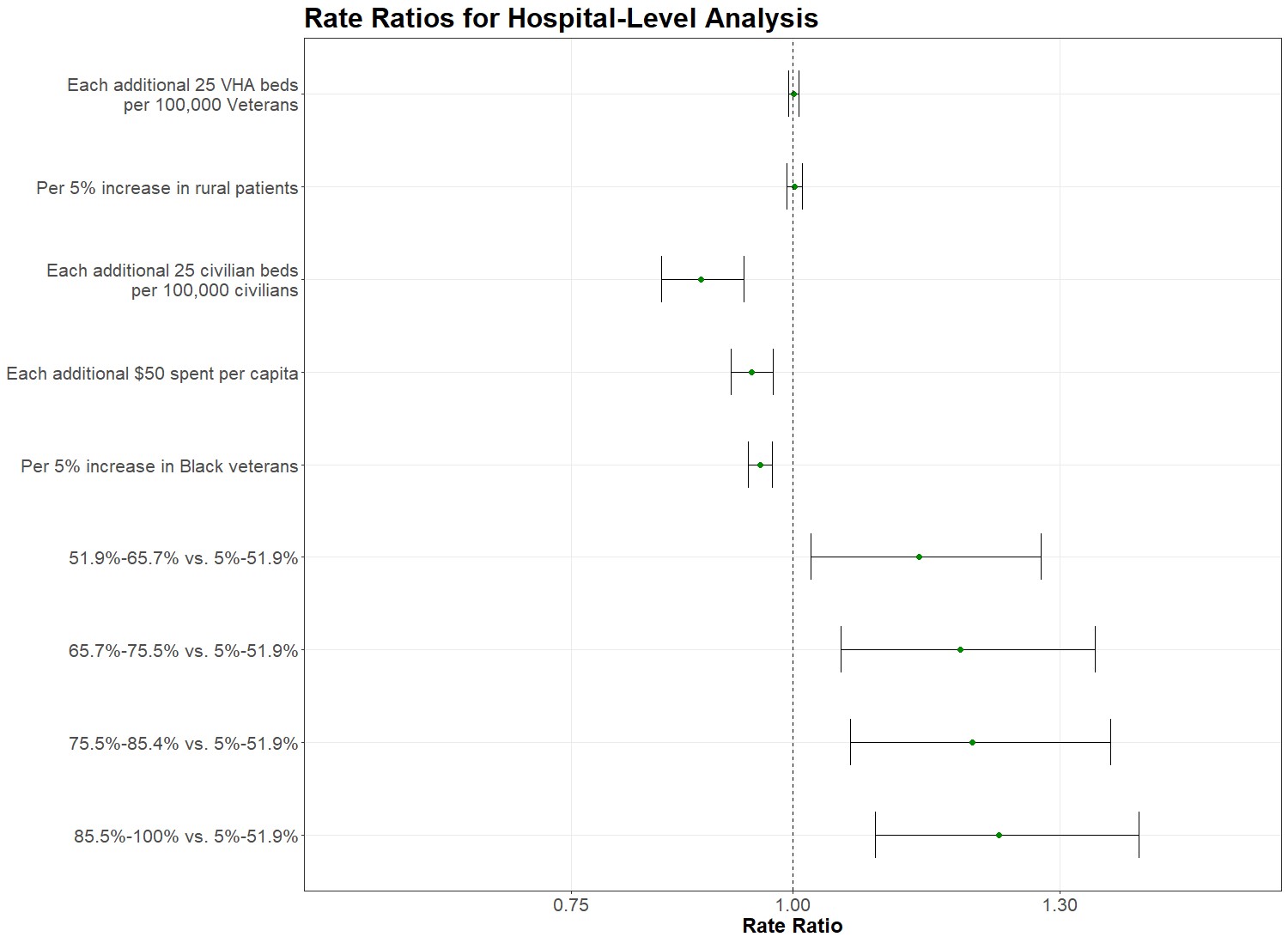
Results: From 2003 to 2016, the rate of veteran suicide has increased while the number of acute mental health beds in VHA hospitals has decreased, per 100,000. (Figure 1) Of 10,119,845 Veterans identified, 26,105 (0.26%) died by suicide. Compared to hospitals in the lowest occupancy quintile, rate ratio (RR) of suicide increased in quintile 2 (RR=1.13; 95% confidence interval [CI] 1.01-1.27), quintile 3 (RR=1.19; 95%CI 1.05-1.34), quintile 4 (RR=1.20; 95%CI 1.06-1.35), and quintile 5 (RR=1.24; 95%CI 1.10-1.41). Of the community-level contextual variables, lower suicide risk was observed for each additional 25 community psychiatric beds/100,000 population (RR=0.89; 95%CI 0.85-0.94) and each additional $50 spent on mental health per capita (RR=0.95; 95%CI 0.93-0.97). (Figure 2)
Conclusions: Lack of acute inpatient psychiatric bed availability in VHA hospitals was associated with higher suicide risk while additional community mental health investment was associated with lower suicide risk. This is the first study to use occupancy data and not just numbers of beds to assess the potential risk of bed availability and suicide. Future work should clarify optimal levels of bed availability and mental health spending to reduce suicide rates.