Background: For hospitalists rounding on inpatient units, admitting new patients at varying times through the day greatly disrupts workflow efficiency. Deferring these admissions to the next shift can result in delays in patient care. Admitting teams dedicated to the needs of new patients offer a potential solution.
Methods: A quality improvement project was conducted on a large adult hospital medicine service in an urban academic medical center. Attending physicians, nurse practitioners, and physician assistants participated. Patterns of admission assignment were tracked over a 16-week period surrounding the intervention.Stakeholders from the frontline clinical staff, hospitalist service leadership, bed management, and capacity command groups were actively engaged in project planning. The project team participated in analysis of the admission process, which identified several targets for improved workflow.The team identified several key drivers of rounding workflow improvement, including reducing overall number of assigned admissions, concentrating admissions in the afternoon hours, and minimizing variability in number of admissions seen by rounding physicians. The specific goal adopted was a reduction of the number of new admissions assigned to rounding hospitalists by 25% over an 8-week period. Change ideas included establishing a team of hospitalist staff dedicated to admitting patients on the day shift, redesigning the admission assignment process, and transferring hospitalist staff resources from the afternoon/evening “swing” shift to the day shift. The hospital medicine service implemented a dedicated admitting team of physicians and advanced practice providers and limited rounding physicians’ admitting responsibilities to defined afternoon time periods. Existing staff resources were shifted from the swing shift to the day shift, avoiding the need to hire new staff for this project. For physicians assigned to rounding on existing inpatients, shift time available for new admissions was reduced from 8-10 hours to 2-3 targeted afternoon hours daily.The outcome metric was number of weekly day shift admissions assigned to rounding physicians. Process metrics included the number of weekly admissions assigned to the new admitting team. Percent of day shift admissions deferred to the night shift was chosen as a balancing metric.
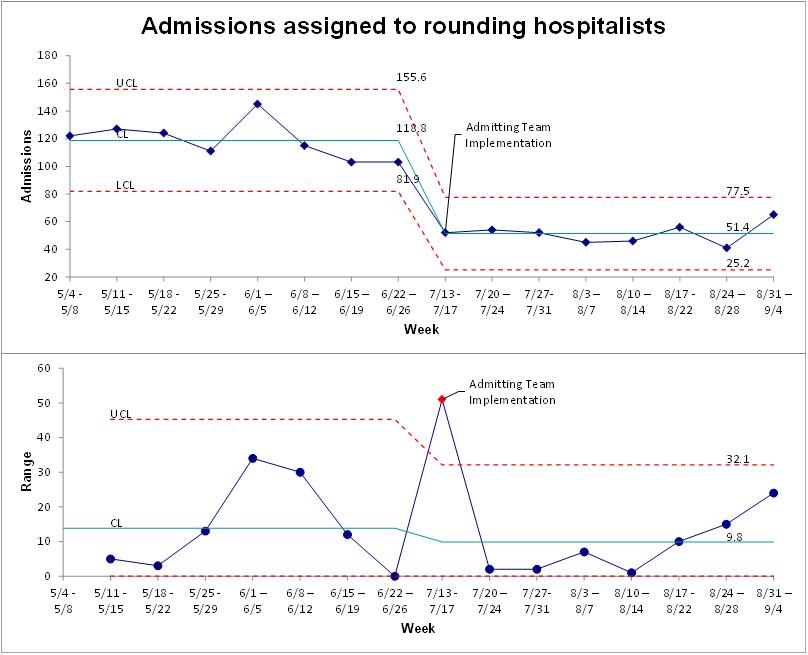
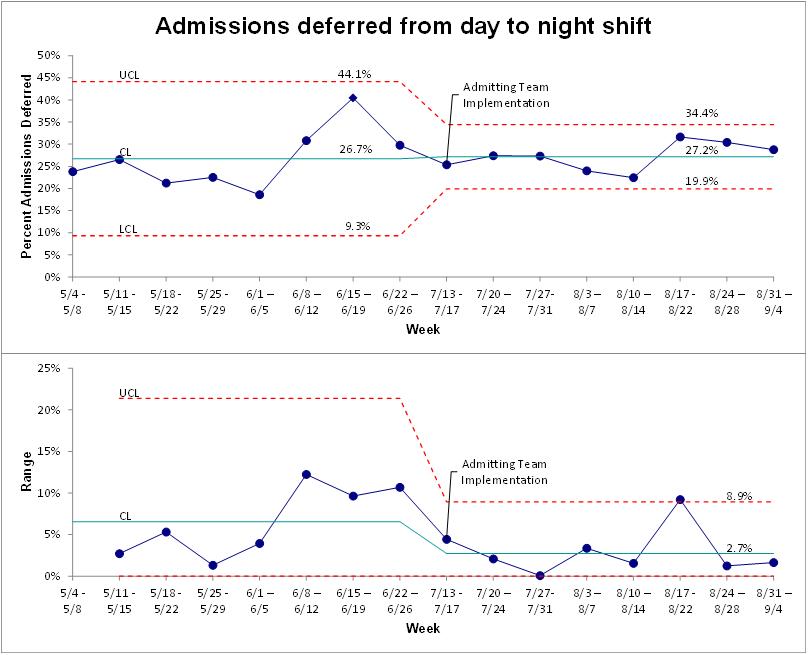
Results: Over the 8 weeks following implementation of the admitting team, mean weekly day shift admissions handled by rounding physicians decreased from 118 to 51 (a 57% absolute reduction) (Fig. 1). The new admitting team was assigned a mean of 99.5 admissions weekly (range 81-114). Mean weekly day shift admissions deferred to the night shift remained unchanged (27.2% vs. 26.7%) (Fig. 2).
Conclusions: Implementation of a team of hospitalists dedicated to new patient admissions was associated with significant reductions in new patient admissions assigned to rounding physicians. Percentage of day shift admissions deferred to the night shift was not impacted by this change. Future work should explore the downstream effects of this intervention including rounding efficiency, patient outcomes, discharge efficiency, length of stay, readmissions, and patient/hospitalist satisfaction.