Background: As the day progresses, clinicians may experience decision fatigue that impairs clinical reasoning. Such impairment may exert its greatest effects on clinicians’ abilities to identify and effectively treat heterogeneous clinical syndromes with high diagnostic uncertainty, including sepsis. We therefore examined the association of time of day with antibiotic initiation among hospitalized ward patients with sepsis.
Methods: In four acute care hospitals of the University of Pennsylvania Health System, we conducted a retrospective cohort study of the first episode of hospital-acquired sepsis for non-ICU patients admitted October 2016 through June 2019. Sepsis onset was defined using CDC Adult Sepsis Event and Sepsis-3 criteria. The exposure was number of hours from the start of the work day, defined as 7AM. First, we fit a discrete-time time-to-event model with hours from sepsis onset as the time axis, to assess the association between hour relative to 7AM and the probability of antibiotic initiation among patients with sepsis. Second, we used logistic regression to assess the association between time of sepsis onset and odds of antibiotic initiation within three hours, as recommended by the CMS SEP-1 quality measure. For both analyses, we adjusted for hospital, admission year, and patient age, gender, race, ethnicity, admitting diagnosis, and service type (medical, surgical).
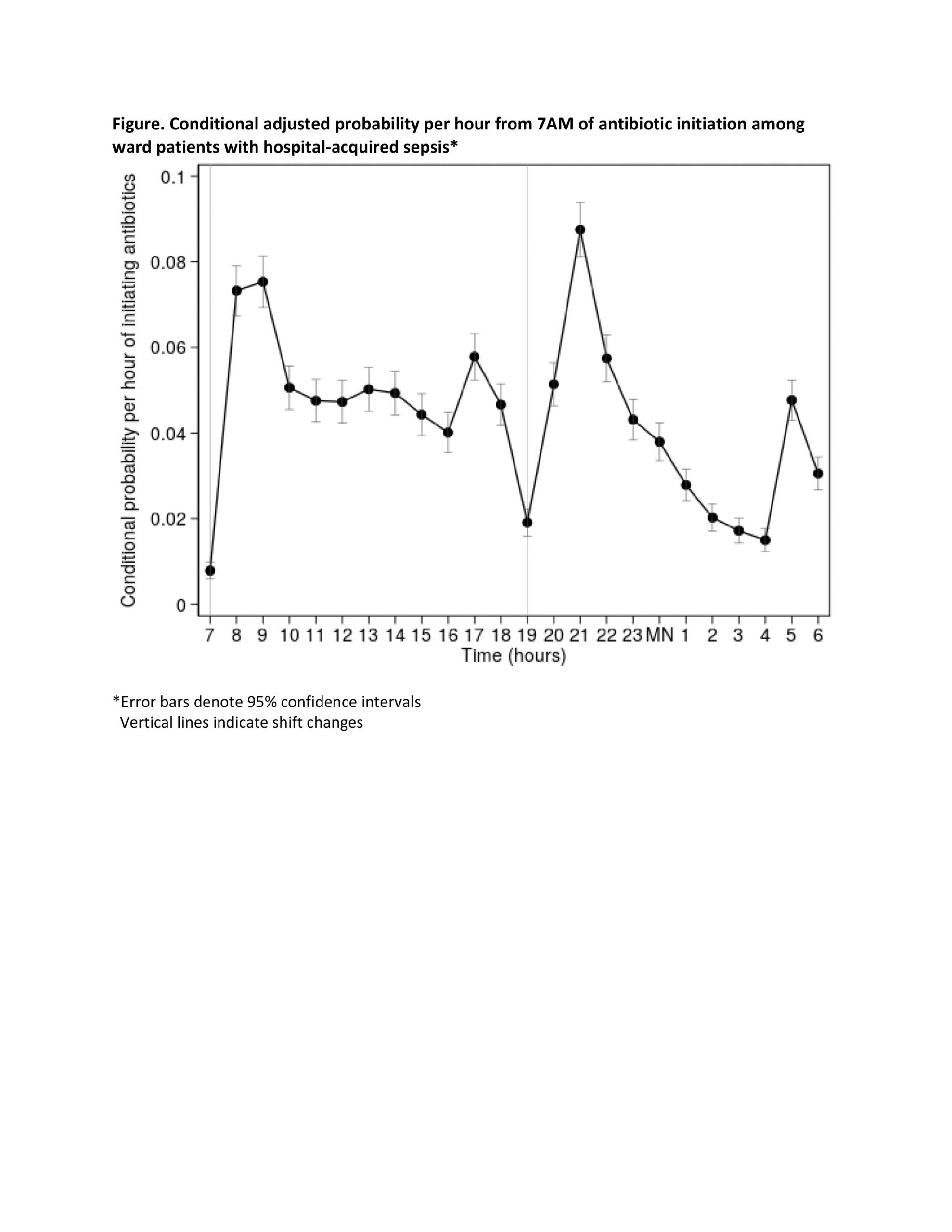
Results: Among 156,399 visits, 7,569 (5%) had a sepsis episode. Median age was 62 years (IQR 51-71), 53% were male, and 79% were on medicine services. Median time to antibiotic initiation was 10 hours (IQR 3-48) after sepsis onset and 2,057 (27%) patients received antibiotics within three hours.Probabilities of antibiotic initiation ranged from 0.8% (95% CI 0.6%-1.0%) at 7AM to 8.7% (95% CI 8.1%-9.4%) at 9PM. Using 7AM as the reference group, the probability of antibiotic initiation at each other hour differed significantly (p<0.001) (Figure). Using 7AM as the reference group for sepsis onset, odds of antibiotic initiation within three hours also differed significantly, ranging from 0.5 (95% CI 0.3-0.7) at 4PM to 1.5 (95% CI 1.0-2.1) at 9PM.
Conclusions: Antibiotic initiation peaks at 9AM and 9PM, early in clinicians’ 12-hour shifts, and subsequently declines throughout these shifts with nadirs at 7AM and 7PM at shift changes. We observed similar patterns for antibiotic initiation within three hours from sepsis onset. These findings suggest that between-shift handoff processes and/or decision fatigue cause delays in treatment for hospitalized patients with sepsis. Confirming these findings and distinguishing between these mechanisms may lead to quality-enhancing interventions.