Background: In-hospital venous thromboembolism (VTE) remains an important preventable cause of morbidity/mortality. Multiple risk assessment models (RAMs) for VTE in hospitalized medical patients have been developed, validated, and endorsed by several national societies. Despite evidence and guidelines supporting risk stratification for VTE prevention, data suggest that prophylactic measures are not appropriately utilized. In a nation-wide clinician survey, we aimed to study attitudes and use of VTE RAMs in hospitalized patients.
Methods: We developed an instrument exploring current attitudes and practices around VTE prophylaxis in adult hospitalized patients, including use of RAMs. The survey was distributed electronically through social media, professional healthcare organizations, and internal medicine program directors across the US. Data collected was reported as proportions with 95% confidence intervals (CI). We used log-binomial regression to calculate risk ratios (RR) and 95% CIs to estimate the likelihood of using RAMs for assessing VTE risk and bleeding risk by training status, practice setting, thrombosis/hemostasis research interest, and time in practice.
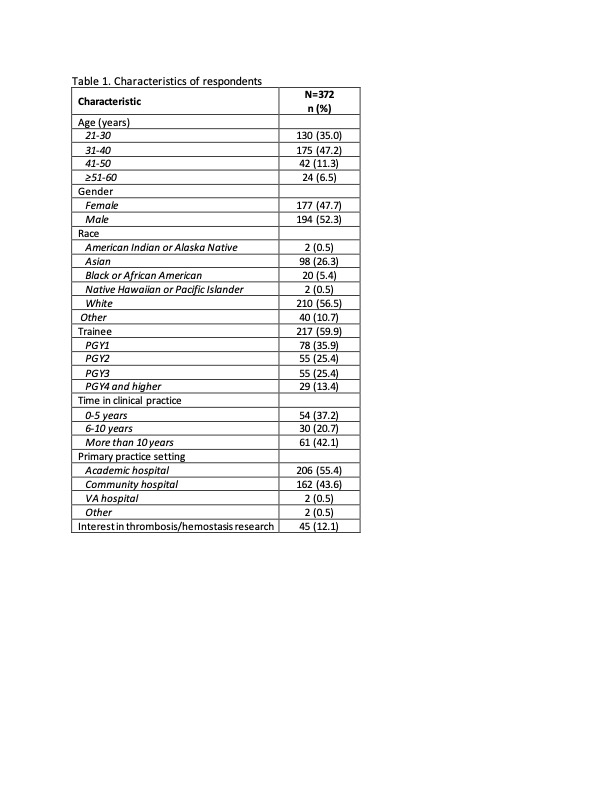
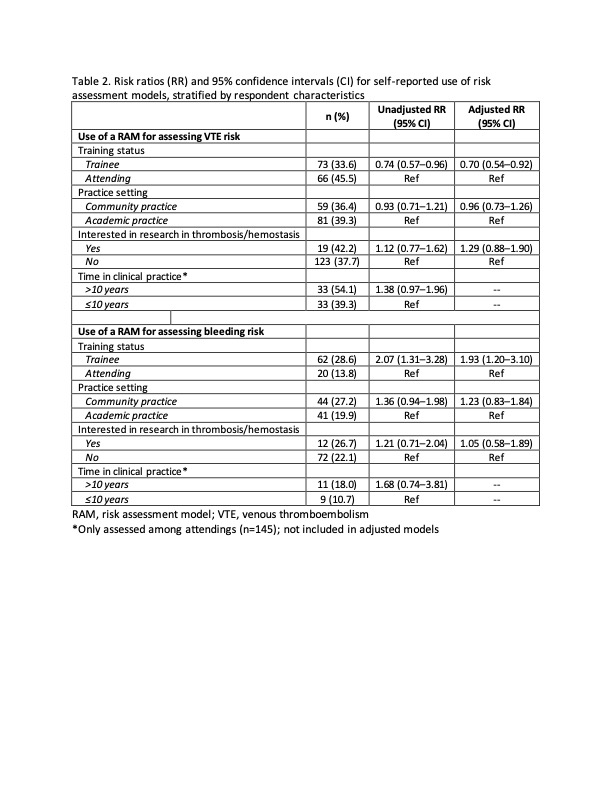
Results: Of 372 respondents, 59.9% were trainees. Overall, 55.4% practiced in an academic hospital, and 43.6% practiced in a community site (Table 1). Almost all respondents agreed that VTE prophylaxis is important for patient care (98.4%, 95% CI: 96.5–99.4) and that current prophylactic measures are safe (91.6%, 95% CI: 88.3–94.3) and effective (94.6%, 95% CI: 91.7–96.6). However, only slightly over half (56.2%) perceived that patients at their own institutions were on appropriate prophylaxis almost all the time. When considering which patients require VTE prophylaxis, only 38.4% of respondents reported using RAMs to determine thrombotic risk, and only 22.9% reported using RAMs to determine bleeding risk. The most commonly cited barriers to utilizing RAMs included not being familiar with their use (50.2%), lack of integration in the electronic medical record (40.2%), and being too time-consuming (17.5%). Of respondents who utilized a RAM, the most commonly reported VTE RAMs used by respondents were the Padua (59.4%) followed by the Caprini (19.6%), and 4-element RAM (15.4%). HAS-BLED was the most commonly used RAM for assessing bleeding risk (85.9%). Trainees were significantly less likely than attending physicians to report using a RAM for risk stratification for VTE (aRR: 0.70, 95% CI: 0.54–0.92), though they were significantly more likely to report use of RAMs to determine bleeding risk (aRR: 1.93, 95% CI: 1.20–3.10; Table 2). There were no other significant differences in the reported use of RAMs for VTE stratification or bleeding risk according to practice site, thrombosis/hemostasis research, or time in training for attending physicians.
Conclusions: In a national survey, in-hospital VTE prophylaxis was deemed important, safe, and effective; however respondents’ perceived rates of institutional use were suboptimal. Only a minority of clinicians reported utilizing RAMs for risk stratification when determining VTE prophylaxis, and RAM use did not differ based on years in practice or site of practice, though it did differ by training status. These data point to suboptimal utilization of VTE RAMs for hospitalized patients and highlight potential strategies to increase use through provider education and integration into electronic systems to enhance efficiency.