Background: Point of care ultrasound (POCUS) significantly augments physical exam and improves medical management, and many medical schools across the United States are implementing undergraduate POCUS curricula. As a result, internal medicine (IM) residency programs have incoming interns with varying levels of POCUS knowledge and skill. We administered a needs assessment questionnaire to incoming interns to evaluate attitudes, confidence, knowledge, and clinical application of POCUS.
Methods: A 57-item survey and knowledge assessment was distributed to 52 interns during intern orientation in June 2017. The survey explored attitudes about POCUS, prior training, and confidence in identifying abnormal POCUS findings. The knowledge assessment assessed baseline knowledge of ultrasound physics, cardiac and pulmonary ultrasound, and clinical application. The content was reviewed by a board-certified cardiologist with specialization in echocardiography and a board-certified pulmonologist. Comparisons between categorical variables were made using Chi-Square and ANOVA tests, and between numeric variables using t-tests. Reliability of the assessment was measured using Cronbach’s alpha. Item analysis was applied to determine item difficulty and discrimination.
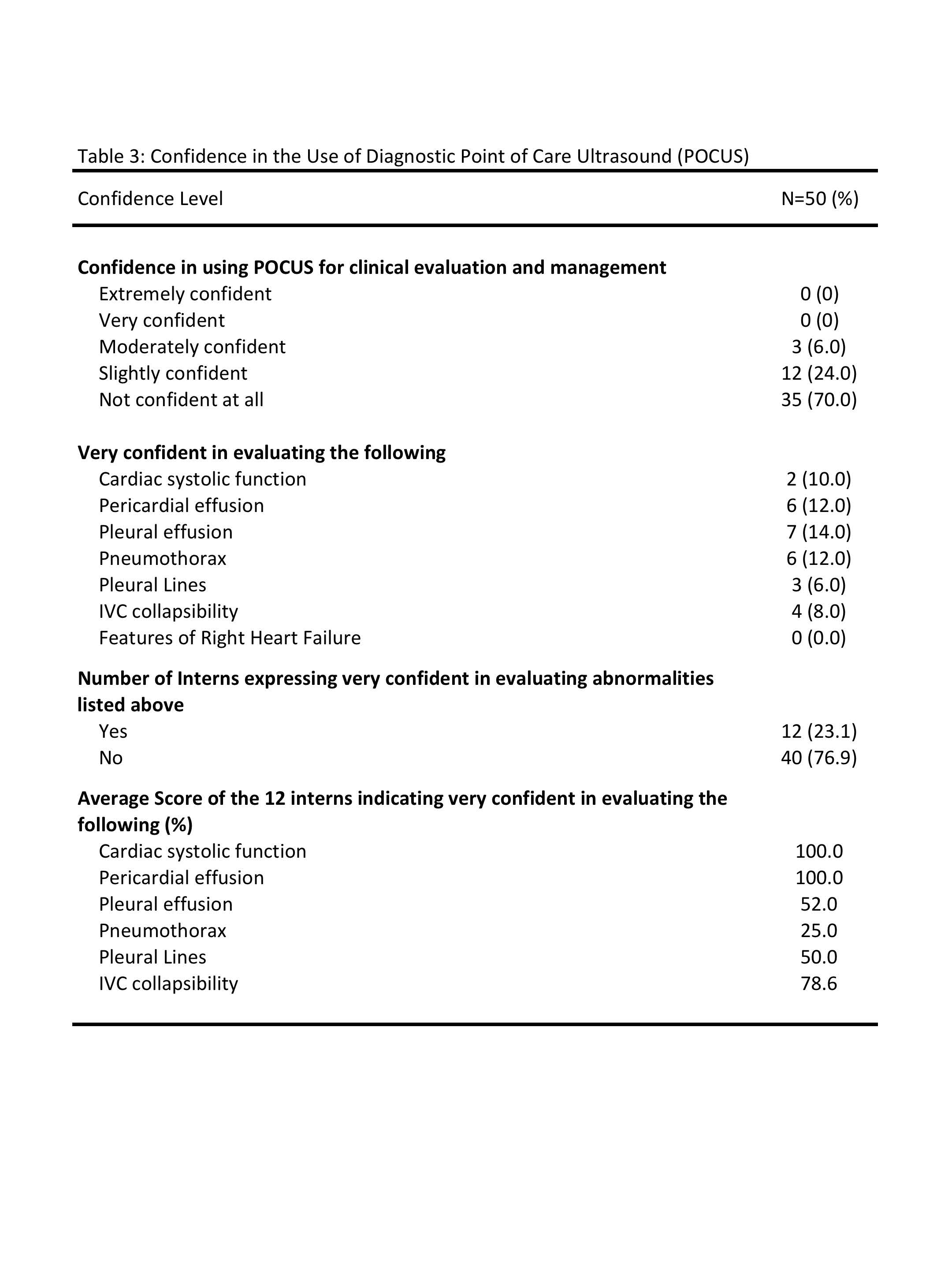
Results: 51 interns completed the assessment. One response was discarded due to delayed completion. Ten percent of interns received some formal training in POCUS during medical school, mostly through ultrasound elective and emergency medicine rotation. Forty-six percent strongly agreed that diagnostic POCUS is an important part of the physical exam and medical management. Although 70% were not confident in using POCUS for clinical evaluation and management, 23.1% expressed high levels of confidence in evaluating abnormal POCUS findings.
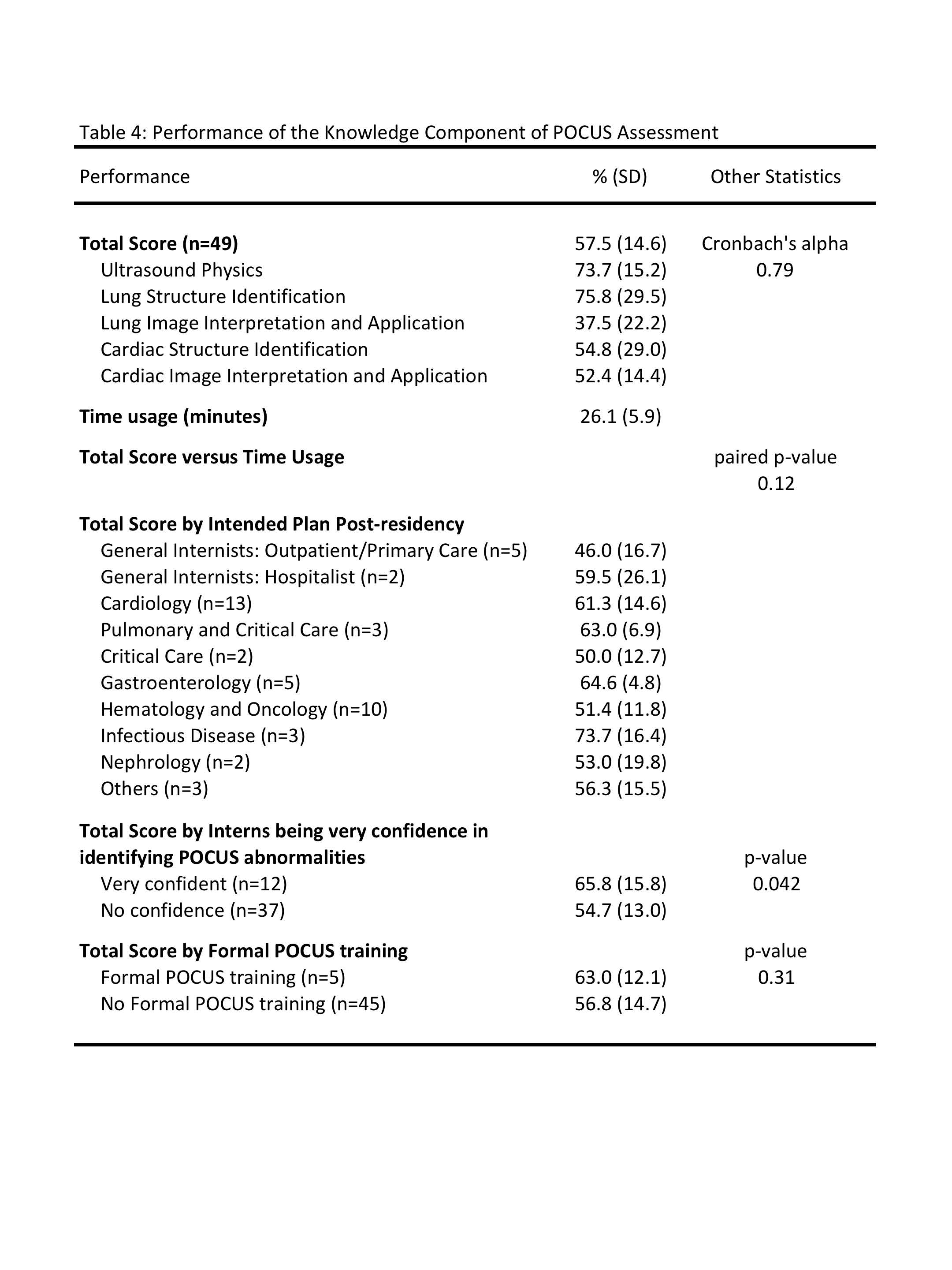
The overall mean on the knowledge assessment was 57.5 (SD 14.4, range 24.0-86.0) with the highest sub-score in structure identification and lowest sub-score in image interpretation and application. There was no statistically significant difference in the total score between interns that received formal ultrasound training and those who did not (63.0, SD 12.1 vs 56.8, SD 14.7; p=0.31). When stratified by level of confidence, interns who were very confident in identifying POCUS abnormalities outperformed those with no confidence (overall score 65.8, SD 15.8 vs. 54.7, SD 13.0; p=0.042). More confident interns recognized systolic function and pericardial effusions accurately, but did not outperform less confident interns in other knowledge areas. The knowledge assessment was highly reliable with a Cronbach’s alpha of 0.79.
Conclusions: This knowledge assessment on cardiac and pulmonary bedside ultrasound was highly reliable. Internal medicine interns express low levels of confidence in their POCUS skills, yet desire at least moderate competence in POCUS skills by the end of residency training. Formal POCUS training during undergraduate medical training did not result in significantly higher overall knowledge scores, or when divided into subcategories. Confidence in identifying abnormal POCUS findings correlated well with performance on knowledge-based questions, but clinical interpretation did not match confidence levels for most skills. These findings reinforce the need to develop formal curricula in POCUS for internal medicine residents with emphasis on image interpretation and clinical application.